Archives of Pulmonology and Respiratory Care
Pulmonary Epithelioid Hemangioendothelioma-Mimicking Mesothelioma
Zeynep Bayramoglu1*, Tolga Semerkant2, Hıdır Esme2 and Yasar Unlu1
2Department of Thoracic Surgery, Konya Training and Research Hospital, Turkey
Cite this as
Bayramoglu Z, Semerkant T, Esme H, Unlu Y (2020) Pulmonary Epithelioid Hemangioendothelioma-Mimicking Mesothelioma. Arch Pulmonol Respir Care 6(1): 030-032. DOI: 10.17352/aprc.000048Pulmoner epithelioid hemangioendothelioma is a rare and multifocal malignant tumor of vascular origin. Patients are generally asymptomatic. Chest pain, cough, weight loss, hemoptysis, and pleural effusion are seen in symptomatic patients. Moreover, it is more common in women. It is difficult to diagnose the patients based on clinical and radiological findings. Histopathological examination is the gold standard. We here aimed to present our pulmonary epithelioid hemangioendothelioma patient pre-diagnosed with mesothelioma when she was admitted to the hospital with dyspnea and had bilateral multiple nodules and bilateral pleural effusion.
Introduction
Pulmonary epithelioid hemangioendothelioma (PEH) is a rare and low-intermediate grade malignant neoplasm of vascular origin [1,2]. PEH is generally asymptomatic. It is more common in women [3]. They are typically seen as multiple partially well-circumscribed nodules on computed tomography (CT) [4]. It is difficult to diagnose PEH based on clinical and radiological findings alone. Histopathological examination is gold standard for the diagnosis of PEH [5]. We here aimed to present a PEH patient transferred to our department with the diagnosis of mesothelioma.
Case report
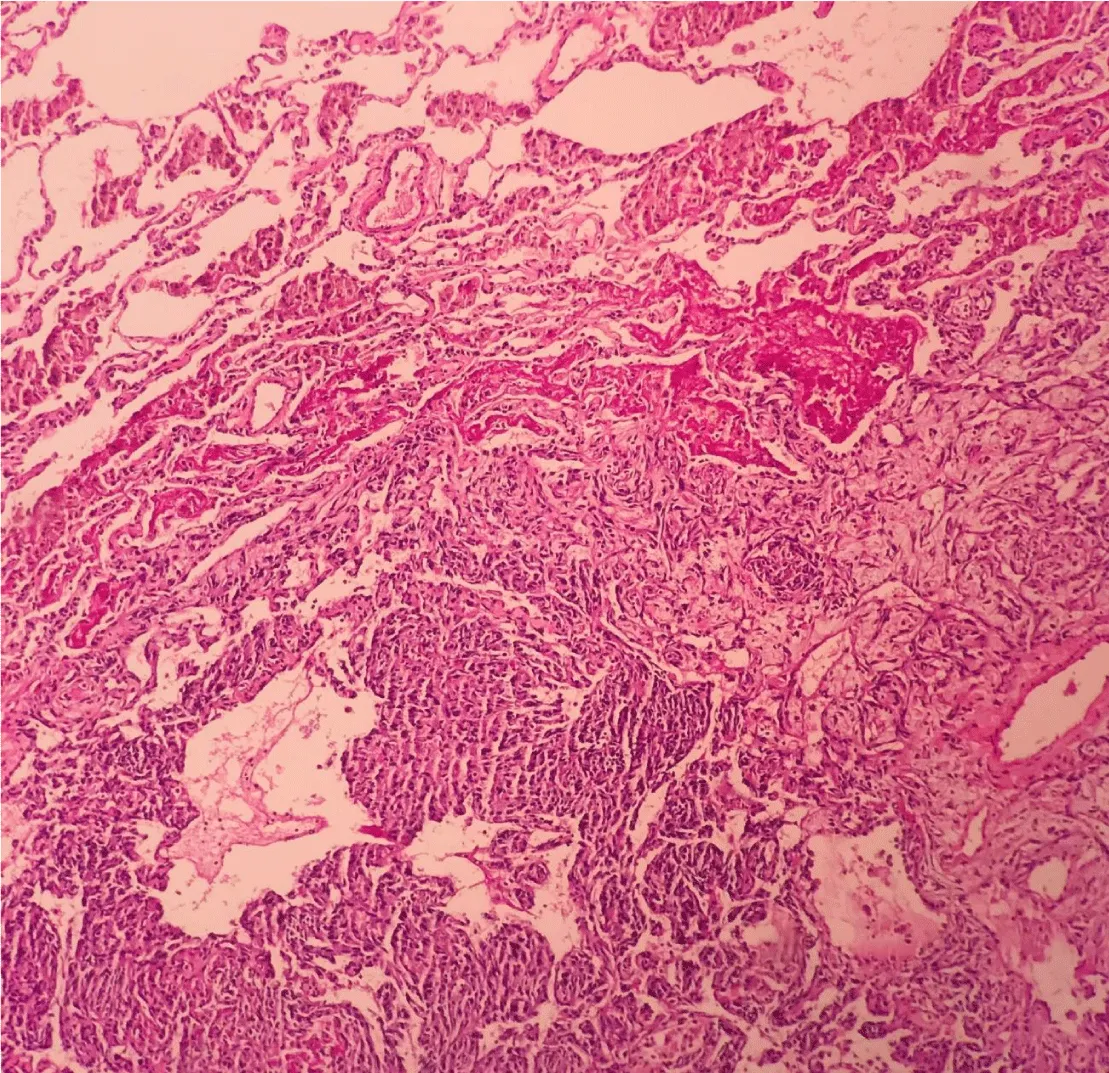
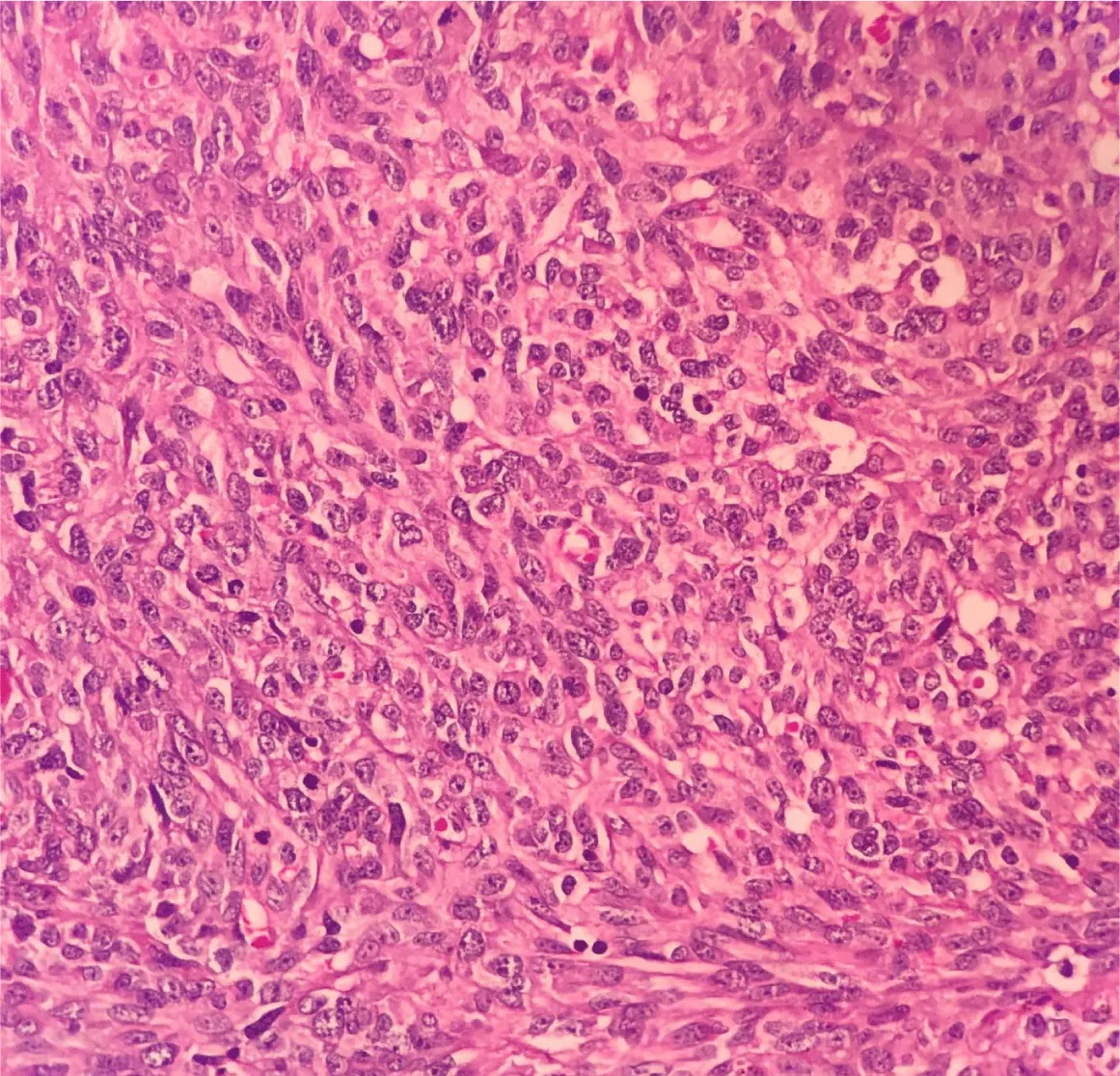
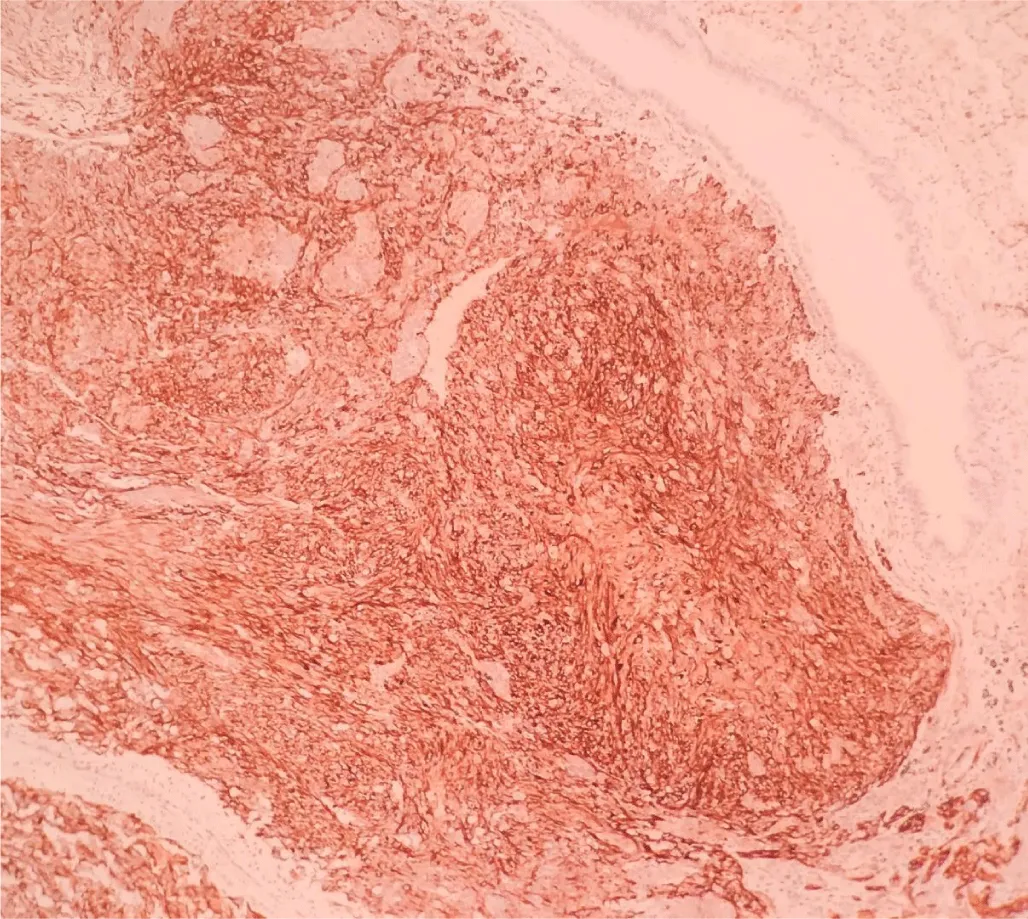
A 40-year-old Syrian woman was admitted to the epicenter of a hospital with shortness of breath lasting for about 1 month. After multiple bilateral nodules were monitored on her CT performed at the epicenter the patient pre-diagnosed with mesothelioma was transferred to our department. In her physical examination: BP: 110/50 mm Hg, PR: 110/min, SpO2: 86% and decreased breath sounds were present at the lung bases bilaterally. She had pleural catheter which was placed to left side at the epicenter. The drain output was 100 cc. PFT FEV1: 0.81 24% and FVC: 0.81 21%. Chest x-ray of the patient showed right sinus blunting, mediastinal widening, bilateral nodular opacities and pleural catheter on the left (Figure 1). On PET-CT scan, there were pleural effusion with 1.76 of SUVmax involvement in bilateral hemithorax and large number of nodules measured as 44 mm in diameter and located on the right upper lobe of the lung and a part of which had hypometabolic and necrotic central area (SUVmax: 1.56). Histopathological examination was recommended as mesothelioma was primarily considered based on PET-CT findings. The patient underwent pleural biopsy with right VATS and wedge resection for pulmonary nodules in upper-middle-lower lobes of the lung. In frozen section, a malignant mesenchymal lesion was reported. That is why the patient underwent pleurodesis. In microscopic examination, epithelioid, rarely fusiform tumor cells were monitored in hyaline matrix in some areas. Cytoplasmic vacuoles were monitored in tumor cells (Figures 2,3). Mild to moderate atypia was observed generally. In immunohistochemical examination, diffusely positive reaction for CD31, CD34, WT-1 and FLI-1 and negative reaction for HHV-8, TTF-1 and ALK were showed (Figures 3-5). The patient was diagnosed with PEH based on histopathological and immunohistochemical findings.
Discussion
PEH was first described as a pulmonary intravascular bronchoalveolar tumor in 1975 [6]. Then, the term ‘Epithelioid Hemangioendothelioma’ (EHE) was used by Weiss and Enzinger in 1982 [7]. Weiss and Enzinger described EHE as a new entity between hemangioma and angiosarcoma. According to the latest WHO classification, EHE was described as low to intermediate grade malignant vascular tumor [1]. EHE can arise in different sites including lung, liver and soft tissue. PEH is a rare tumor and generally seen in young adults. It is two times more common in women [3]. Patients are generally asymptomatic. Chest pain, cough, weight loss, hemoptysis and pleural effusion are seen in symptomatic patients. Some clinicians have proposed three main CT patterns in patients with PEH: multiple pulmonary nodules, multiple pulmonary reticulonodular opacities, and diffuse infiltrative pleural thickening [8,9]. Approximately 160 patients with PEH have been reported worldwide until now.
Metastases, primary lung cancer, lymphoid tumors, benign or malignant vascular tumors, infections, sarcoidosis, and mesothelioma should be considered in radiological differential diagnosis. As our patient had both bilateral multiple pulmonary nodules and bilateral pleural effusion mesothelioma was primarily considered.
In a recent study, it has been reported that WWTR1-CAMTA1 fusion was present in most of EHEs and that this fusion was present in most of classical epithelioid hemangioendothelioma regardless of their clinical behaviors [10]. Therefore, they suggested that additional genetic abnormalities could be responsible in driving more aggressive course in EHE. In this study, overall survivals of EHE patients with WWTR1-CAMTA1 fusion and EHE patients with YAP1-TFE3 fusion were compared [10]. According to the results, patients with conventional EHE in whom WWTR1-CAMTA1 fusion was present had a less favorable outcome compared to the ones in whom YAP1-TFE3 fusion was present and the 5-year overall survival rates in these patients were 59% and 86% respectively [10].
There is no standard treatment for PEH as it is rare. Moreover, tumor resection should be considered for the patients who can endure surgery. The rate of 5-year overall survival is approximately 60% in patients who undergo surgery [11]. Chemotherapy is preferred for patients with a disseminated disease, however, radiotherapy has been proved to be ineffective [12,13].
- Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JH, et al. (2015) The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10: 1243-1260. Link: https://bit.ly/3bY2acq
- Lau K, Massad M, Pollak C, Rubin C, Yeh J, et al. (2011) Clinical patterns and outcome in epithelioid hemangioendothelioma with or without pulmonary involvement: insights from an internet registry in the study of a rare cancer. Chest 140: 1312-1318. Link: https://bit.ly/2XjecIe
- Rojas-Vigott R, Castro CM, Méndez SR (2016) P2. 24: Pulmonary-Epithelioid Hemangioendothelioma: A Case Report of Spontaneous Regression: Track: Supportive Care and Others. J Thorac Oncol 11: S231-S232. Link: https://bit.ly/2XigsiY
- Liu K, Xie P, Peng W, Zhou Z (2014) The computed tomographic findings of pulmonary epithelioid hemangioendothelioma. La Radiol Med 119: 705-713. Link: https://bit.ly/2AKAoDg
- Shao J, Zhang J (2014) Clinicopathological characteristics of pulmonary epithelioid hemangioendothelioma: A report of four cases and review of the literature. Oncol Lett 8: 2517-2522. Link: https://bit.ly/3cPUiLk
- Dail D (1975) Intravascular bronchioloalveolar tumor. Am J Pathol 78: 6a-7a.
- Weiss SW, Enzinger F (1982) Epithelioid hemangioendothelioma a vascular tumor often mistaken for a carcinoma. Cancer 50: 970-981. Link: https://bit.ly/3bVReMy
- Mesquita RD, Sousa M, Trinidad C, Pinto E, Badiola IA (2017) New insights about pulmonary epithelioid hemangioendothelioma: review of the literature and two case reports. Case Rep Radiol 2017. Link: https://bit.ly/3gaNBFH
- Sakamoto N, Adachi S, Monzawa S, Hamanaka A, Takada Y, et al. (2005) High resolution CT findings of pulmonary epithelioid hemangioendothelioma: unusual manifestations in 2 cases. J Thorac Imaging 20: 236-238. Link: https://bit.ly/2Zu7MZo
- Rosenbaum E, Jadeja B, Xu B, Zhang L, Agaram NP, et al. (2020) Prognostic stratification of clinical and molecular epithelioid hemangioendothelioma subsets. Modern Pathology 33: 591-602. Link: https://go.nature.com/3e3yJXQ
- Bagan P, Hassan M, Barthes FLP, Peyrard S, Souilamas R, et al. (2006) Prognostic factors and surgical indications of pulmonary epithelioid hemangioendothelioma: a review of the literature. Ann Thorac Surg 82: 2010-2013. Link: https://bit.ly/2WT2NzF
- Ye B, Li W, Feng J, Shi JX, Chen Y, et al. (2013) Treatment of pulmonary epithelioid hemangioendothelioma with combination chemotherapy: report of three cases and review of the literature. Oncol Lett 5: 1491-1496. Link: https://bit.ly/2WTirer
- Van Kasteren M, Van der Wurff A, Palmen F, Dolman A, Misere J (1995) Epithelioid haemangioendothelioma of the lung: clinical and pathological pitfalls. Eur Respir J 8: 1616-1619. Link: https://bit.ly/2zZ647K
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
