Archive of Urological Research
Case report of gangrenous cystitis in a post-partum female
Jha Prabhat1*, Joshi Bijendra Dhoj2 and Jha Binit Kumar3
2MS General Surgery, Associate Professor, Department of Surgery, Kathmandu Model Hospital, Nepal
3MS General Surgery, Department of Surgery, National Academy of Medical Sciences, Kathmandu, Nepal
Cite this as
Prabhat J, Dhoj JB, Kumar JB (2019) Case report of gangrenous cystitis in a post-partum female. Arch Urol Res 3(1): 005-008. DOI: 10.17352/aur.000005Background: Gangrenous cystitis is an extremely rare condition with very few cases reported in literature. Diagnosis is often delayed due to the nonspecific symptoms. A multidisciplinary team approach and surgical debridement is usually required for management.
Case presentation: This case reports a 27 year old female who developed gangrenous cystitis post-partum. She was managed with partial cystectomy and primary closure of urinary bladder.
Conclusion: Gangrenous cystitis is a condition with high morbidity and mortality. A high index of suspicion is necessary for diagnosis.
Abbreviations
Cumm: Cubic Millimetre; Fr: French; Gm: Gram; L: Litre; MS: Master of Surgery; U/L: Unit/Litre
Background
Gangrenous cystitis is a very rare condition in current medical practice due to the widespread use of antibiotics. Since a review in 1934 of 209 cases, only 30 cases have been reported in the literature [1]. Diagnosis is often delayed due to the nonspecific symptoms such as fever, pain abdomen, and sepsis with features of peritonitis [2-4]. These factors contribute to the high morbidity and mortality of 35% [2-4]. Different direct and indirect factors have been implicated in the pathogenesis [5]. Diagnosis is suspected during cystoscopy and usually confirmed on laparotomy. Management requires a multidisciplinary approach involving urologist, surgeon, gynecologist, and intensivist. Management involves debridement of the necrotic urinary bladder tissue with urinary diversion if necessary.
Case Presentation
A 27 year old Hindu female presented to the emergency department of Alka Hospital on the seventh post-partum day. She had delivered a 4.1 Kilogram male child with good apgar score by spontaneous vaginal delivery. There was history of prolonged labour of 15 hours duration. Both mother and baby were discharged the next day. Her antenatal period was uneventful. She had complaints of abdominal distension, pain abdomen, blood in urine, vomiting and no passage of stool for 4 days.
On presentation to the emergency patient was hypotensive with blood pressure 90/50 mmHg, tachycardic with pulse rate 114/minute and tachypnoiec. She was maintaining saturation of 98% with oxygen via face mask. On chest examination bilateral basal crepitation were heard. Abdomen was distended with diffuse tenderness. Bowel sound was absent. Foley’s catheterization was done which drained 50 mL of hemorrhagic urine. Investigations showed increased total white blood cell count 29,900/cumm, creatinine 1.6 mg%, hemoglobin 15.9 gm%, platelet 1,93,000/cumm. Ultrasound scan of abdomen showed diffuse collection in peritoneal cavity.
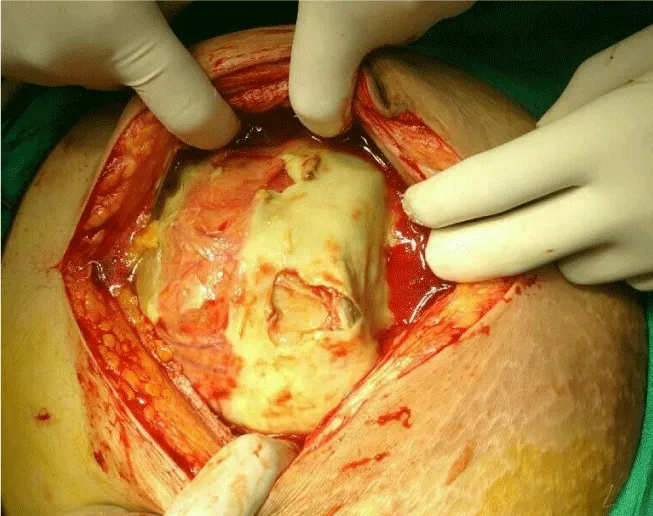
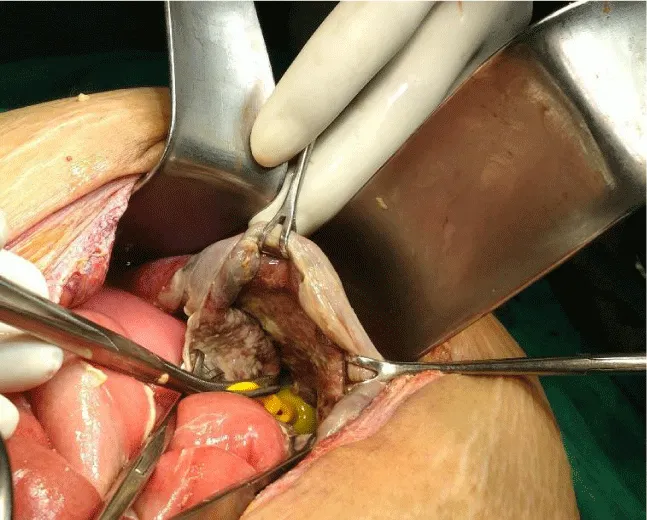
Patient was started on broad spectrum antibiotics meropenem and levofloxacin, nasogastric tube was inserted and laparotomy was planned. Rigid cystoscopy in the operation theatre was done which showed sloughed out urinary bladder mucosa. The per-operative findings on laparotomy was pyoperitoneum with dense interloop collection approximately 5 L (Figure 1). The urinary bladder was flabby and gangrenous with 10 cm perforation at dome with sloughed out mucosa (Figure 2). Trigone was spared. Peritoneal lavage with debridement of necrotic bladder tissue was done. Bilateral ureteric catheters (6 Fr) were placed and pulled out through urethral meatus. Closure of urinary bladder was done with absorbable suture in two layers. Abdomen was closed over a Bogota bag.
Patient was transferred to intensive care unit. She was extubated the next day and started on total parenteral nutrition. Nasogastric tube was removed on 3rd post-operative day and patient was started on oral feeds. Albumin was infused for hypoalbuminemia. Daily dressing was done. On the 5th post-operative day patient developed right sided consolidation with pleural effusion. Ultrasound guided tapping of the fluid revealed exudative effusion with LDH 2536 U/L, protein 1.2 gm%. It was managed with broad spectrum antibiotics, chest physiotherapy.
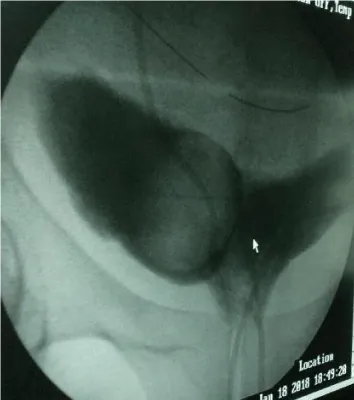
Patient underwent excision of Bogota bag with tension suturing of abdomen on 9th post-operative day. Intraoperative cystogram didn’t show any leak from urinary bladder (Figures 3,4). Ureteric catheters were removed on the 10th post-operative day. On the 15th post-operative day chest X ray revealed multiloculated pleural effusion for which chest tube was inserted. Chest tube was removed on day 5 and patient was discharged the next day. Tension sutures were removed on 21st day. Patient is doing well on follow up.
Discussion
Gangrene of urinary bladder is a rare condition [1]. Few cases have been reported since the advent of antibiotics and improved medical and obstetric care [2-4]. Cristol and Greene have categorized the etiology of this condition into direct and indirect causes [5]. Different direct and indirect factors have been implicated. Common direct factors include chemicals, radiation or widespread infection which produces cellular death of vesical mucosa. Indirect factors interfere with blood supply leading to bladder ischemia & hence gangrene. These include over distension of bladder secondary to chronic urinary retention, pressure of malpositioned pregnant uterus, prolonged labour, pelvic malignancies or blockage of arterial or venous channels by infection, emboli or thrombophlebitis [5,6].
The cause in this case was prolonged labour and overdistension of bladder. Rai et al., reported a case of gangrenous cystitis in a woman following vaginal delivery [6]. The cause was prolonged labour. Stalin Viswanathan et al., reported a case of emphysematous cystitis in a postpartum patient following a vacuum delivery [7].
In the few sporadic cases that have been reported during recent time’s iatrogenic causes such as pelvic radiation [8], pelvic surgery [9] and the use of chemotherapeutic agents [10-12], predominate. Other causes such as infection, urinary retention, and pelvic thrombophlebitis and colovesicals fistulae have also been reported [13-15].
The common clinical presentation are fever, dysuria, hematuria, pyuria or sepsis and peritonitis. Urinary retention due to pus or exfoliated debris in urine is common. Diagnosis is usually made by history, examination and on laparotomy for peritonitis. Our patient also presented with similar symptoms.
Management requires a multidisciplinary team approach involving surgeon, urologist, gynecologist, and anaesthesiologist. Surgical treatment with laparotomy and debridement of necrotic bladder tissue with urinary diversion is required in most cases. Hiney et al., reported a case of gangrenous cystitis in a 83 year old women who underwent total cystectomy and bilateral ureterocutaneostomy. The causative factor was overdistension [16]. Fujiwara et al., described a 74 year old woman who developed panperitonitis due to bladder gangrene. The patient underwent total cystectomy with bilateral ureterocuteneostomy [17].
Conclusion
Gangrenous cystitis is a very rare condition occurring post-partum. A high index of suspicion is required for diagnosis. A multidisciplinary team approach and emergency surgery is required for management. Timely diagnosis and aggressive management can reduce morbidity and mortality.
Declarations
Consent to publish
Consent was taken from the patient and patient party for publication of this report.
The authors would like to thank the patient and patient party who stood tough and gave permission for the publication of this case report.
Funding
All costs incurred during the collection of data and preparation of this manuscript have been covered by the authors.
Availability of data and materials
The patient information are available for review.
Competing interests
1. The authors’ would like to disclose that the interpretation of data or presentation of information in this manuscript hasn’t been influenced by their personal or financial relationship with other people or organizations.
2. The authors haven’t received reimbursements, fees, funding, or salary from an organization that may in any way gain or lose financially from the publication of the article, either now or in the future.
3. The authors aren’t holding stocks or shares in an organization that may in any way gain or lose financially from the publication of the article, either now or in the future.
4. The authors aren’t holding, or currently applying for, patents relating to the content of the manuscript.
5. The authors aren’t receiving reimbursements, fees, funding, or salary from an organization that holds or has applied for patents relating to the content of the manuscript.
Authors’ contributions
PJ and BDJ carried out the conception and design of the study. PJ and BDJ acquired the data. BKJ, BDJ and PJ analyzed and interpreted the data. BDJ critically revised the manuscript and gave the final approval. All authors read and approved the final manuscript.
- Striling WC, Hopkins GA (1934) Gangrene of the bladder. Review of 207 cases and report of 2 personal cases. J Urol 3: 517-525. Link: https://tinyurl.com/yxu3p7s8
- Hinev A, Anakievski D, Krasnaliev I (2010) Gangrenous cystitis: report of a case and review of the literature. Urol Int 85: 479-481. Link: https://tinyurl.com/y3exegmx
- Viswanathan S, Rajan RP, Iqbal N, Subramani J, Muthu V (2012) Enterococcus faecium related emphysematous cystitis and bladder rupture. Australas Med J 5: 581-584. Link: https://tinyurl.com/y68e56p5
- Charra B, Hachimi A, Sodki M, Gueddari H, Benslama A, et al. (2008) Urinary peritonitis caused by gangrenous cystitis. Signa Vitae 3: 32-33. Link: https://tinyurl.com/y5vrkdra
- Cristol DS, Greene LF (1945) Gangrenous cystitis. Surgery 18: 343-346. Link: https://tinyurl.com/y4r8pap2
- Rai R, Sikka P, Aggarwal N, Shankaregowda SA (2015) Gangrenous Cystitis in A Woman Following Vaginal Delivery: An Uncommon Occurrence - A Case Report. J Clin Diagn Res 9: QD13- QD14. Link: https://tinyurl.com/yxwur7v6
- Viswanathan S, Rajan RP, Iqbal N, Subramani J, Muthu V (2012) Enterococcus faecium related emphysematous cystitis and bladder rupture. Australas Med J 5: 581-584. Link: https://tinyurl.com/y68e56p5
- Sataa S, Habiba M, Emna M (2013) Urinary peritonitis caused by gangrenous cystitis. La tunisie Medicale 91: 736-737. Link: https://tinyurl.com/y6quuxub
- Devitt AT, Sethia KK (1993) Gangrenous cystitis: case report and review of the literature. J Urol 149: 1544-1545. Link: https://tinyurl.com/y3cfryqh
- Daines SL, Hodgson NB (1969) Spontaneous rupture of a necrotic bladder. J Urol 102: 431-433. Link: https://tinyurl.com/y66wksw9
- Marsh FP, Vince FP, Pollock DJ (1971) Cyclophosphamide necrosis of bladder causing calcification, contracture and reflux; treated by colocystoplasty. Br J Urol 43: 324-332. Link: https://tinyurl.com/yxuu29hd
- Engel WJ, McCormack LJ (1958) Acute necrotizing angiitis of the bladder; report of a case. J Urol 79: 230-236. Link: https://tinyurl.com/y5zyfvgf
- Mihatsch MJ, Ohnacker H, Herzog B (1974) Bladder necrosis caused by use of THAM in a newborn infant. J Urol 111: 835-837. Link: https://tinyurl.com/y6xyvm72
- Charra B, Hachimi A, Sodki M (2008) Urinary peritonitis caused by gangrenous cystitis. Signa Vitae 3: 32-33. Link: https://tinyurl.com/y5vrkdra
- Schmidt SS (1995) Gangrene of the bladder due to over distention. J Urol 153: 409-410. Link: https://tinyurl.com/yyfngho5
- Hinev A, Anakievski D, Krasnaliev I (2010) Gangrenous cystitis: report of a case and review of the literature. Urol Int 85: 479-481. Link: https://tinyurl.com/y3exegmx
- Fujiwara S, Noguchi T, Noguchi T, Emoto A, Tasaki Y (2008) Panperitonitis caused by gangrene of the urinary bladder: report of a successfully treated case. Am Surg 74: 302-304. Link: https://tinyurl.com/y567tako
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
