Archive of Urological Research
Decubitus positioning, a free method to allow access, organ protection in thermal ablation and exclusion of liver involvement of an anterior cortex renal tumour
Tan Zehao1*, Teo Jin Kiat2, Terence Lim Say Kiat2, Poh Wee Teng3 and Ng Keng Sin1,4
2Department of Urology, Changi General Hospital, Singapore
3Department of Laboratory Medicine, Changi General Hospital, Singapore
4Diagnostic Imaging, Mount Alvernia Hospital, Singapore
Cite this as
Tan Z, Teo JK, Lim TSK, Poh WT, Ng KS (2020) Decubitus positioning, a free method to allow access, organ protection in thermal ablation and exclusion of liver involvement of an anterior cortex renal tumour. Arch Urol Res 4(1): 073-075. DOI: 10.17352/aur.000023Renal tumours are getting detected earlier and smaller owing to increase in imaging volume with renal cell carcinoma as one the top 10 most common cancer in Singapore. With ageing population, this is expected to be seen in patients with multiple co-morbidities raising challenges for surgical management.
Exclusion of hepatic invasion by renal tumours in the anterior cortex is usually difficult. Access for biopsy and ablation of renal tumours at the anterior cortex is also an issue with trans-hepatic, retroperitoneal approaches risking injury to the liver and posterior aspect of the kidney and an anterior trans-peritoneal approach risking bowel perforation and tract seeding.
The liver is an intra-peritoneal organ while the kidney is retroperitoneal. With this anatomical knowledge, we present a case which uses decubitus positioning to provide path for access, organ protection and to exclude hepatic involvement. This is free and serves as an example for cost saving measure in an economy of rising healthcare cost due to an aging population.
Introduction
Owing to increased cross-sectional imaging, more renal tumours are getting detected incidentally earlier and smaller. Renal cell carcinoma (RCC) is the 9th most common cancer in male population in Singapore [1] with T1a (i.e. < 4 cm) tumours accounting for more than half of the RCCs at diagnosis [2]. For small renal tumours, thermal ablation should be offered according to the latest position statement by the society of interventional radiology [3].
Given the aging population in Singapore with resulting rising healthcare costs [4], it is expected that a portion of these patients would have significant co-morbidities. These often precludes or make surgical management a challenge. For such patients, minimally invasive treatment such as thermal ablation is an option and would be expected to increase in volume.
Access of the renal tumours at the anterior aspect of the right kidney are particularly difficult both for biopsy and ablation as the liver is in the way. The right kidney is closely related to right lobe of the liver at the bare area. For a tumour at the anterior upper to interpolar region of the kidney, direct invasion of renal tumours into the liver though uncommon and only shown in several case reports [5,6] can pose as a diagnostic dilemma.
We describe a case which decubitus positioning of the patient excluded hepatic invasion and provided a window for percutaneous transperitoneal biopsy and ablation of a small renal tumour.
Case presentation
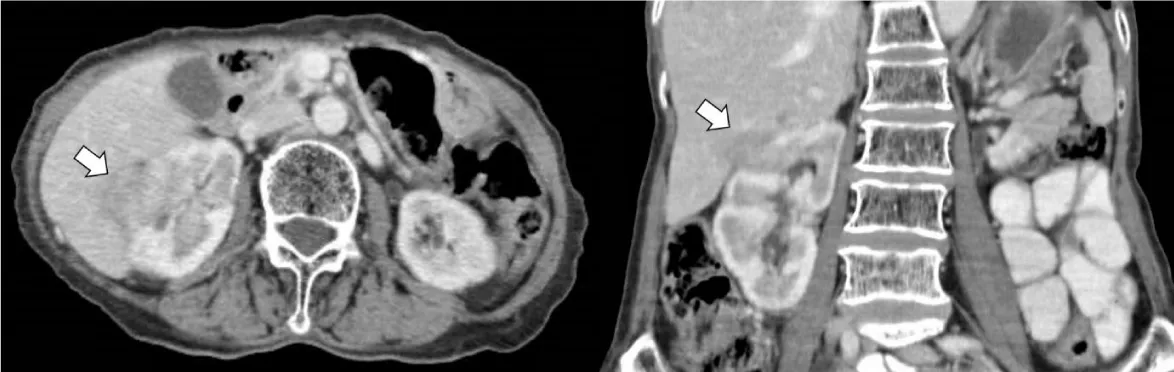
Our patient is a 71 years old female who was found to have an incidental solitary 2.7 cm enhancing renal tumour arising from right upper pole on a surveillance scan for gastric cancer. The patient had a past history of gastric resection followed by radiotherapy for positive perigastric adenopathy. There was no evidence of local and distant metastases on the same examination. The renal tumour was inseparable from segment VII of the liver at the bare area (Figure 1). After discussion at the multi-disciplinary team meeting, decision was made for percutaneous biopsy to obtain histological diagnosis as the differentials were RCC or renal metastasis with possible invasion of the liver.
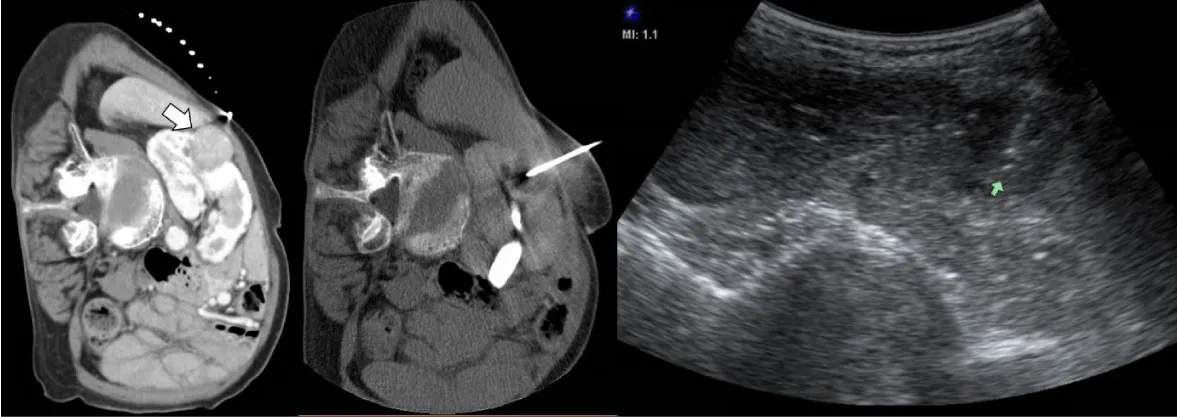
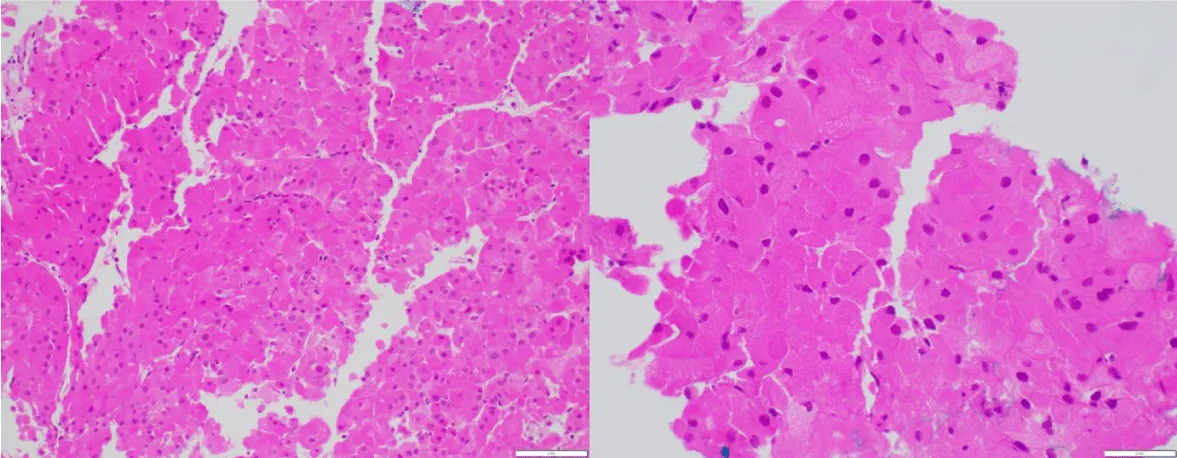
The patient was placed on right side up decubitus position during contrast enhanced computed tomography (CT), which confirmed the renal tumour was separate from the liver. Percutaneous biopsy was performed under ultrasound and CT guidance. Images taken during percutaneous biopsy are shown in Figure 2. The tumor demonstrates immunoreactivity to AMACR, Vimentin, CAM 5.2 (diffuse in oncocytic cells and focal in pale cells), CK7 (focal), E-Cadherin (focal) CD10 (focal); RCC antigen (focal). It is non -immunoreactive to Hepar-1 (Figure 3). Given definitive differentiation from other renal tumour subtypes is not feasible, decision was made to for thermal ablation of this tumour.
The position of the tumour at the right anterior abdomen also provided a window for transperitoneal percutaneous access. After hydrodissection with 150 mls of 5% dextrose solution to separate the renal tumour from the liver, the renal tumour was ablated using a 15 cm long CoolTip (Coviden, Dublin, Ireland) radiofrequency ablation needle with a 3 cm active tip for 12 minutes. Tract ablation was also performed. Figure 4a demonstrates transperitoneal approach to ablation. Adequate ablation was achieved on immediate post-procedural CT without evidence of bowel perforation. Follow up contrast enhanced CT in 1 year showed no evidence of local recurrence or evidence of tract seeding (Figure 4b).
Discussion
Considerations in deciding on the approach to biopsy and ablation of tumour at the anterior upper to interpolar region of the kidney predominantly focuses on avoiding critical structures (i.e. adequate organ protection). On supine positioning, an anterior trans-hepatic approach requires traversing a large amount of hepatic parenchyma while a posterior retroperitoneal approach traverses a significant portion of renal parenchyma. Since both of these are highly vascular organs, these approaches should be avoided when possible to prevent significant bleeding. More inferior transperitoneal approach may be carried out on supine positioning but would risk of injuring the large amount of bowel loops anteriorly and peritoneal seeding when transgressing the peritoneal space [7,8].
A myriad of organ protection techniques have been developed to prevent organ injury during thermal ablation, these include hydrodissection, balloon interposition and electrode torqueing [9]. However, patient positioning is a simple and free but often ignored way of organ protection to allow displacement of critical structures and the target organ from each other allowing a shorter and clearer path of access.
Since the liver is an intra-peritoneal organ and the kidneys are retro-peritoneal organs, these are mobile relative to each other. Knowledge of this allowed the use of decubitus positioning to separate the liver and kidneys which in conjunction with hydrodissection to displace the anterior bowel loops provided a window for a short tract of entry along the anterior abdominal wall. This also enabled us to achieve adequate ablation without complications such as bleeding, bowel perforation or tract seeding as minimal transgression of the free intra-peritoneal space.
Decubitus positioning of abdominal CT is not commonly done particularly to troubleshoot diagnostic dilemma. The utility of decubitus positioning was twofold for our patient. Besides facilitating access, it allowed separation of the liver from the right kidney which enabled confident exclusion of hepatic invasion of the renal tumour, an important diagnosis to make as hepatic invasion herald a grave prognosis [5] and limited percutaneous intervention.
As alluded to previously, patients with small renal tumours might have more co-morbidities owing to aging population and increased detection. This will likely lead to an increased volume for minimally invasive therapy such as thermal ablation. Our case demonstrates usage of anatomical knowledge, to achieve improved outcomes. There is no additional cost and it should be utilized more frequently to curb escalating healthcare costs.
Conclusion
With an aging population, minimally invasive therapy of renal tumours is expected to be more common. Imaging guided percutaneous ablative therapy may require expertise in displacement of adjacent organs to prevent collateral damage. Renal tumours in the anterior aspect of the right kidney can be difficult to access and protect for percutaneous thermal ablation.
Our case illustrates that with anatomical knowledge, a simple method of placing the patient on decubitus positioning with trans-peritoneal approach allows a twofold utility for thermal ablation of anterior renal tumour with enabling access to allow organ protection, prevent seeding and exclude hepatic invasion. This also serves as an example of a method to reduce healthcare costs.
- National Registry of Diseases (2020) Singapore Cancer Registry 50th Anniversary Monograph 1968-2017 (2013-2017 mortality data): Singapore Cancer Registry.
- Volpe A, Panzarella T, Rendon RA, Haider MA, Kondylis FI, et al. (2004) The natural history of incidentally detected small renal masses. Cancer 100: 738-745. Link: https://bit.ly/3jqLgqI
- Morris CS, Baerlocher MO, Dariushnia SR, McLoney ED, Abi-Jaoudeh N, et al. (2020) Society of Interventional Radiology Position Statement on the Role of Percutaneous Ablation in Renal Cell Carcinoma: Endorsed by the Canadian Association for Interventional Radiology and the Society of Interventional Oncology. Journal of Vascular and Interventional Radiology. 31: 189-194.e3. Link: https://bit.ly/37Rd990
- Low LL, Kwan YH, Ko MSM, Yeam CT, Lee VSY, et al. (2019) Epidemiologic Characteristics of Multimorbidity and Sociodemographic Factors Associated With Multimorbidity in a Rapidly Aging Asian Country. JAMA Netw Open 2: e1915245. Link: https://bit.ly/37L2aOI
- Johnin K, Nakai O, Kataoka A, Koizumi S, Dok An C, et al. (2001) Surgical management of renal cell carcinoma invading into the liver: radical nephrectomy en bloc with right hepatic lateral sector. Urology 57: 975. Link: https://bit.ly/3kw4cpq
- Fujii M, Kamimura T, Tsukino H, Furukoji E, Sakae T, Yano K, et al. (2018) Safe Resection of Renal Cell Carcinoma with Liver Invasion Using Liver Hanging Technique Supported by Preoperative Portal Vein Embolization. Case Rep Urol 2018: 5139034. Link: https://bit.ly/2TtLy5C
- Park BK, Kim CK (2009) Complications of image-guided radiofrequency ablation of renal cell carcinoma: causes, imaging features and prevention methods. Eur Radiol 19: 2180-2190. Link: https://bit.ly/3oyWqh0
- Wah TM, Irving HC, Gregory W, Cartledge J, Joyce AD, et al. (2014) Radiofrequency ablation (RFA) of renal cell carcinoma (RCC): experience in 200 tumours. BJU Int 113: 416-428. Link: https://bit.ly/2TpC0IM
- Ginat DT, Saad WE (2010) Bowel displacement and protection techniques during percutaneous renal tumor thermal ablation. Tech Vasc Interv Radiol 13: 66-74. Link: https://bit.ly/2TwtnvS
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
