Open Journal of Orthopedics and Rheumatology
A mesenchymal chondrosarcoma of the right tibia in a young man requires disarticulation of the right knee: A case study
Youness Mokhchani1,2*, Abderrafia Rachdi1,2, Abdelhay Rabbah1,2, Jalal Boukhriss1,2, Bouchaib Chafry1,2 and Mustapha Boussouga1,2
2Faculty of Medicine and Pharmacy, Mohammed V University-Rabat-10000, Morocco
Cite this as
Mokhchani Y, Rachdi A, Rabbah A, Boukhriss J, Chafry B, et al. (2022) A mesenchymal chondrosarcoma of the right tibia in a young man requires disarticulation of the right knee: A case study. Open J Orthop Rheumatol 7(1): 004-007. DOI: 10.17352/ojor.000043Copyright License
© 2022 Mokhchani Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Chondrosarcoma is a malignant tumor occupying the 2nd position in terms of frequency, all ages combined, after osteosarcoma [1]. Epidemiological data extracted from cancer registries in Europe indicate an annual incidence of ~0.1/100,000 inhabitants [2]. Mesenchymal chondrosarcoma of bone is a rare high-grade variant of chondrosarcoma (2-13%), which usually has an extra-skeletal (30-40%) or central intramedullary location (15-30%). It is very rare for this tumor to grow on the surface of a long bone. Unlike conventional and dedifferentiated chondrosarcoma which have a male predominance (between 40-60 years old), this variant affects both men and women indiscriminately and rather affects young populations between 20 and 30 years old, but cases have been described in children. Or the elderly [3-6]. Chondrosarcomas are known to be radio-chemo-resistant. Radiotherapy and chemotherapy can be used for tumors that cannot be removed surgically, in addition to conservative surgery, or in the event of recurrence. Surgery is the mainstay of treatment. All the authors recommend wide excision passing into the healthy zone (one-piece resection). The possible surgical procedures are curettage followed by cryotherapy or filling with surgical cement; conservative surgery with reconstruction by bone and skin grafts or placement of an endoprosthesis; and finally amputation. The latter is recommended when there is vascular-nervous invasion, large tumor, or local recurrence after conservative surgery. Most people who have an amputation will wear an artificial limb (prosthesis) after surgery [7-12]. We describe a patient with mesenchymal chondrosarcoma appearing in the middle third of the right tibia for which radical surgery was instituted.
He is a 24-year-old young man who came to our hospital with a history of pain and swelling in the front part of his leg that had been evolving for a year and gradually increasing in volume and which had been neglected by the patient and his entourage at the beginning. The patient is a young engineering school graduate, weighing 75kg, measuring 1.8m, BMI= 23.15kg/m2. The patient could walk without any assistance. On examination, there was a firm mass painful on palpation, 10*4cm at the level of the middle third of the right tibia, with painful skin facing it, brownish in color. Ranges of motion of the right knee and ankle were normal. The sensitivity and motor skills of the right lower limb including the right ankle were preserved, without any deficit. Peripheral pulses were present. Examination of other systems was unremarkable.
Faced with this clinical picture, a standard radiograph was performed, which showed a heterogeneous lacuna at the level of the right tibial diaphysis (Figure 1). This assessment was completed by Magnetic Resonance Imaging (MRI) which objectified a suspicious process in the midshaft region of the right tibia, measuring 124*63*51mm, with an upper pole located 8.5 cm from the tibial plateau (Figure 2). Following these radiological data, a surgical biopsy was performed to clarify the histological nature of the tumor. The anatomopathological examination came back in favor of a mesenchymal chondrosarcoma (this variant is still considered grade 3 “high grade”). A staging assessment was performed including a thoraco-abdominopelvic Computed Tomography (CT) scan which was unremarkable, and a Positron Emission Computed Tomography with 18 FDG which showed just the tumoral process with no other focus (no metastases) (Figure 3).
Given the very aggressive nature of the tumor, in particular, the vasculonerve invasion, and given the failure of the three courses of chemotherapy that the patient has already received in another hospital (no documents), and the impossibility of performing oncological surgery, the indication for radical surgery (amputation) was taken, but the patient delayed the surgical act because he was initially opposed to this indication. The goal of our treatment was to save the patient first of all and to have a stump that could easily be fitted with a principle of keeping as much length as possible, minimizing the risks and skin lesions, and finally maintaining the patient's autonomy. To do so, disarticulation of the knee was an excellent alternative before considering amputation of the thigh, since it is a quick procedure, with little bleeding, allows excellent terminal support without ischial support, is easy of fitting, and is less energy-intensive. In addition, several studies have shown that disarticulation of the knee according to "Gritti-Stokes" allows for faster equipment, shorter rehabilitation, as well as all the functional parameters, which are superior compared to amputation of the thigh [13-14].
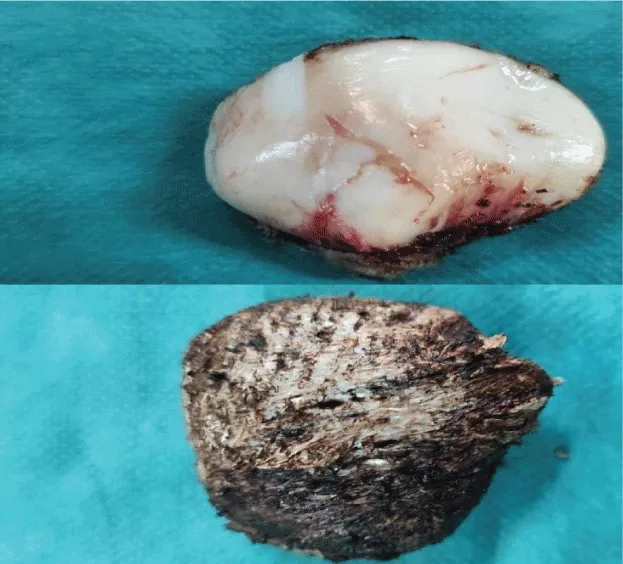
Before the surgical procedure, the patient was seen and followed by a psychologist for support and psychological preparation for the intervention. The latter took place under locoregional anesthesia in the supine position, and after a shark's mouth incision (Figure 4), the disarticulation was performed in a conventional manner. The patella was enucleated from the extensor apparatus (Figure 5), then the patellar tendon was sutured to the remnants of the anterior cruciate ligament. The gastrocnemius muscles were sectioned 15 cm from their proximal insertions, thus bypassing the femoral condyles to be sutured to the anterior wall (Figures 6,7). Finally, the closure was plane by plane on the suction Redon drain, while positioning the scar behind, away from the support zone (Figure 8).
The postoperative course was simple, the patient was put on antibiotics for 48 hours, analgesics, and anticoagulants. The patient stayed in our service for 20 days for the daily control of the dressing and the scar. The management of the postoperative phase was multidisciplinary, in collaboration with the psychologist, physiotherapist, and orthoprosthetist. Its aim was to allow socio-professional reintegration of the patient, and the resumption of physical activities (sport, leisure, etc.). After the healing, we started with the toning of the stump and the muscular reinforcement to fight against amyotrophy, the maintenance of the articular amplitudes (of the two hips, the contralateral knee, and ankle), the reinforcement of the muscles of the contralateral lower limb to supplementing the amputated lower limb, strengthening the muscles of the upper limbs to allow crutching, and finally improving unimodal balance and proprioception. Then we continued by teaching the patient to put on and take off his prosthesis while controlling his hygiene, then we proceeded to his walking training with a prosthesis with a foam sleeve, while gradually increasing the wearing time of the prosthesis to gradually gain endurance. Rehabilitation was strewn with various problems that delayed its progress (skin problems, poor adaptation of the prosthesis, phantom pain, etc...). With each incident, modifications were made to the equipment by the orthoprosthetist.
The evolution after a year and a half of follow-up is favorable without any skin problems or pain, and the patient can walk using a comfortable and aesthetic prosthesis. The check-up revealed no local recurrence or metastasis.
- Parvizi J, Kim GK. Chapter 49 - Chondrosarcoma. In: Parvizi J, Kim GK, editors. High Yield Orthopaedics. Philadelphia: W.B. Saunders. 2010; 100-1.
- Hogendoorn PC; ESMO/EUROBONET Working Group, Athanasou N, Bielack S, De Alava E, Dei Tos AP, Ferrari S, Gelderblom H, Grimer R, Hall KS, Hassan B, Hogendoorn PC, Jurgens H, Paulussen M, Rozeman L, Taminiau AH, Whelan J, Vanel D. Bone sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010 May;21 Suppl 5:v204-13. doi: 10.1093/annonc/mdq223. PMID: 20555083.
- Streitbuerger A, Gosheger G, Hardes J. Chapter 35 - Chondrosarcoma of bone: diagnosis and therapy. In: Heymann D, editor. Bone Cancer (Second edition). San Diego: Academic Press; 2015; 415-424.
- Gelderblom H, Hogendoorn PC, Dijkstra SD, van Rijswijk CS, Krol AD, Taminiau AH, Bovée JV. The clinical approach towards chondrosarcoma. Oncologist. 2008 Mar;13(3):320-9. doi: 10.1634/theoncologist.2007-0237. Erratum in: Oncologist. 2008 May;13(5):618. PMID: 18378543.
- Kim MJ, Cho KJ, Ayala AG, Ro JY. Chondrosarcoma: with updates on molecular genetics. Sarcoma. 2011;2011:405437. doi: 10.1155/2011/405437. Epub 2011 Feb 15. PMID: 21403832; PMCID: PMC3042668.
- Gorlick RG TJ, Marina N. Chondrosarcoma. In: Kufe DW, Pollock RE, Weichselbaum RR, et al., editors. Holland-Frei Cancer Medicine. 6th edition. Hamilton (ON): BC Decker; 2003.
- American Cancer Society. Bone Cancer. 2016.
- Gerrand C, Athanasou N, Brennan B, Grimer R, Judson I, Morland B, Peake D, Seddon B, Whelan J; British Sarcoma Group. UK guidelines for the management of bone sarcomas. Clin Sarcoma Res. 2016 May 4;6:7. doi: 10.1186/s13569-016-0047-1. PMID: 27148438; PMCID: PMC4855334.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Bone Cancer (Version 1.2017). 2016.
- O'Donnell RJ, Dubois SC, Hass-Kogan DA. Sarcomas of bone. DeVita VT Jr, Lawrence TS, Rosenberg SA. Cancer: Principles and Practice of Oncology. 10th ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2015; 91:1292-1313.
- Samuel LC. Bone and soft-tissue sarcoma. Yarbro CH, Wujcik D, Holmes Gobel B (eds.). Cancer Nursing: Principles and Practice. 8th ed. Burlington, MA: Jones and Bartlett Learning; 2018; 46:1243-1277.
- Streitbuerger A, Gosheger G, Hardes J . Chondrosarcoma of bone: diagnosis and therapy. Heyman D, (ed). Bone Cancer: Primary Bone Cancer and Bone Metastases. 2nd ed. San Diego, CA: Academic Press; 2015: 35: 415–424.
- Taylor BC, Poka A, French BG, Fowler TT, Mehta S. Gritti-stokes amputations in the trauma patient: clinical comparisons and subjective outcomes. J Bone Joint Surg Am. 2012 Apr 4;94(7):602-8. doi: 10.2106/JBJS.K.00557. PMID: 22488616.
- Campbell WB, Morris PJ. A prospective randomized comparison of healing in Gritti-Stokes and through-knee amputations. Ann R Coll Surg Engl. 1987 Jan;69(1):1-4. PMID: 3566109; PMCID: PMC2498432.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
