Archives of Organ Transplantation
A case of high drain output after renal transplantation: Review of current evidence
Sajid Mohmad1,2, Ajay Sharma2,3 and Ahmed Halawa2,4*
2Faculty of Health and Life Science, Institute of Learning and Teaching, University of Liverpool, UK
3Royal Liverpool University Hospitals, Liverpool, UK
4Sheffield Teaching Hospitals, Sheffield, UK
Cite this as
Mohmad S, Sharma A, Halawa A (2018) A case of high drain output after renal transplantation: Review of current evidence. Arch Organ Transplant 3(1): 001-005. DOI: 10.17352/2640-7973.000010Surgical complications are not uncommon after renal transplantation. They should always be in the differential diagnosis of renal graft dysfunction. While ruling out or confirming a surgical cause of graft dysfunction, a sequential approach should be undertaken starting from clinical examination and moving on to more invasive investigations as the clinical picture becomes clearer. Biochemical assay of drain fluid is important. Causes of a collection around/near the graft include abscess, hematoma, urinoma and lymphocele. Treatment of each of them is different.
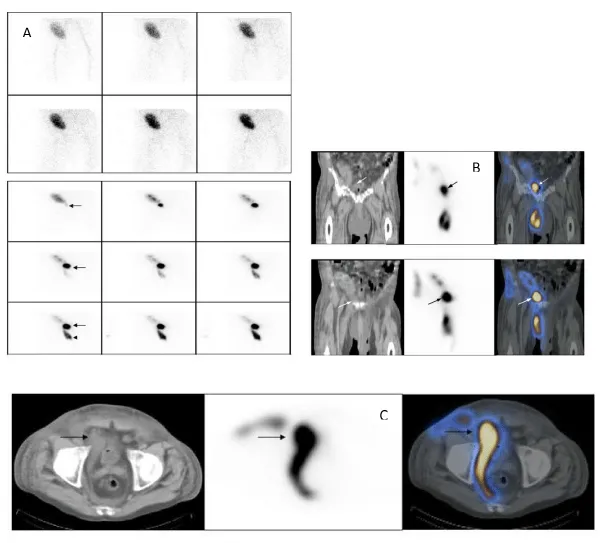
Causes of urinoma can be donor derived or surgical technique related. SPECT/CT may be needed to confirm the location of urinary leak. Treatment of the urinoma depends on its severity and location. Small and distal lesions can be treated conservatively while as larger and proximal leaks need surgical intervention. Ureteric stenting may be undertaken as a prophylaxis against urinary leak.
Lymphoceles should always be considered as a cause of perinephric collection in renal transplant. It can be differentiated from a urinoma by the concentration of creatinine in the drain fluid. The treatment may be conservative or surgical depending on the size of the lymphocele and initial response or resistance to conservative management.
Scenario: A 28-year-old CKD 5 underwent a kidney transplantation from his brother with primary function. Post-surgery, the drain is quite productive (820 mls on day 2 and 750 mls on day 3). Drain fluid biochemistry showed K of 28 mmol/L and creatinine of 16000 μmol/l. His serum creatinine on that day was 416 μmol/l and serum K is 5.1 mmol/L.
Introduction
Surgical complications remain common causes of renal transplant dysfunction in early post transplant period. Any patient with a renal graft dysfunction should be evaluated for surgical complications including collections. Investigations should be tailored individually to each patient. Correlation of clinical examination and laboratory evaluation is fundamental for diagnosis in such cases. Biochemical assay of the drain fluid and radiological examination are essential.
Common causes of collection around transplanted kidney are hematoma, urinoma, lymphocele and abscess.
In this review, we discuss different causes of collections after a renal transplant, their diagnosis and management.
Scenario
The index patient is a renal transplant recipient day 3 post living donor renal transplant with productive drain (820 mls on day 2 and 750 mls on day 3). Drain fluid biochemistry has showed K of 28 mmol/L and creatinine of 16000 μmol/l. His serum creatinine on that day was 416 μmol/l and serum K is 5.1 mmol/L.
The approach to this case should be orthodox, starting with physical examination looking for any pre-renal causes of creatinine not falling as expected. The fluid charts should also be reviewed. The patient should be given fluids if they are not volume overloaded.
When evaluating delayed graft function or slowly falling creatinine in a recipient, root cause needs to be evaluated. The causes are either donor or recipient derived (ischemic injury, donor type, vascular injuries etc). Delayed graft function is traditionally defined as the use of dialysis within seven days of the transplant [1].
The second step would be to perform a scan to rule out or confirm urinary obstruction, to check perfusion and look for any collections. Serum and drain fluid should be sent simultaneously for biochemistry if needed.
The likely causes of a collection and dysfunction in early post renal transplant period are urinoma, hematoma/haemorrhage, lymphocele or abscess (Table 1). These pathologies can generally be differentiated from each other by examination of the drained fluid. While hematoma fluid will have high hemoglobulin concentration, the fluid from an abscess will have high white blood cell count and a urinoma fluid would be positive for high creatinine.
Urinoma
The risk factors for urinary complications post transplant are male recipient, black recipient and U stitch technique of the ureteral anastomosis [2]. Ureteric complications are more likely after donation after cardiac death (DCD) than after living donation or donation after brain death (DBD) though donor type is not a risk factor [3]. In addition, urinary leak may be lower after ureteroureterostomy as compared to ureterocystostomy [4].
Urinary leakage makes up around 1/4th of all urological complications [5], which occur at a rate of around 3 – 6% after renal transplantation [3-5].
Urinary leakmay present clinically with a picture of peritonitis if the urine is present in peritoneal cavity in case of an intraperitoneally placed kidney. More commonly, swelling around the graft or high drain output may be the only sign. In some cases, it may present as a swelling of the ipsilateral lower limb.
Causes
The major cause of urinary leak is ureteral necrosis and devascularisation during organ harvest. However, there are other causes of urinary leak like technical failure including a poor construction of the ureterocystostomy resulting in a non-watertight anastomosis, dehiscence or polar artery ligation. Depending upon the cause, the urinary leak may present within 24 hours if secondary to technical error or after 2 weeks if secondary to necrosis [6].
Diagnosis
Biochemical – The drain fluid is six times more likely to be secondary to urine leak compared to lymphocele if the drain creatinine is 6 times higher than the plasma creatinine and the urine creatinine is not more than 3 fold drain creatinine and is 7 times higher than the plasma creatinine [7]. It is noteworthy that drained fluid from the urine leak may have creatinine nearer to plasma if creatinine clearance is low.
Radiological – Ultrasonography helps in identifying a collection around or near the renal graft. However, it may be difficult to differentiate urinoma from other collections. Usually, urinoma is a well-defined simple collection without internal echoes while as abscesses and hematomas are hyperechoic with septations. A urinoma may show septations if it is secondarily infected or blood contaminated.
In some cases diagnosis may still be unclear. Scintigraphic99mTc-DTPArenography may play an important role in such cases especially if the volume of urine leak is large. The pattern of photopenia and its course over time may differentiate urine leak from lymphocele, hematoma and abscess. The initial photopenic region which becomes hotter than the background is very likely secondary to a urine leak as compared to other causes [8].
Scintigraphy is more sensitive than ultrasonography in the diagnosis of urinoma. AyşegülDirlik et al reported five patients who underwent imaging related to collection around the graft. Ultrasound diagnosed urinary leak in one patient out of four while as scintigraphy detected all the four cases of urinary leak in addition to one false positive [9].
Even after confirming that the collection is secondary to a urine leak, the exact location of the leak may still be undetected. Accompanying SPECT/CT may be very useful in evaluating the anatomy of the urine leak [10], (Figure A-C).
Treatment
Stenting: ureteral stenting is used routinely after renal transplantation. The contribution of stents in preventing urine leaks is controversial.
In this prospective randomized study [11], with a total of 194 renal transplant patients, 97 were randomized to have a double pigtail stent inserted and another 97 patients were without a stent. 6 patients in the no-stent group had urinary leak while only one patient in the stent group developed a urinary leak, hence favouring stenting.
In another randomized trial, 280 renal transplant recipients were randomized to either a no-routine stent group or a routine stent group. In the no-routine stent group patients were not stented except for an intra-operative event based on surgeon’sopinion. There was no difference between the groups in an intention to treat analysis [12].
The approach to the management of urinary leak is either conservative or surgical. The surgical exploration is undertaken if the urine leak is large and/or proximal and if the conservative management has failed previously.
Conservative management includes urinary diversion and is usually considered in small distal urine leak. Urine is diverted by placing a Foley’s catheter and a percutaneous nephrostomy tube. If the urinomas are large, they should be drained surgically. The nephrostomy may help determining the anatomy of urinary leak. The tubes are removed once leak resolves. Nephrostography should be performed regularly as surveillance for the urine leak and to check closure.
In one study the documented closure rate was 87% with infection related complications occurring in 17% and one case of stricture [13]. Balloon dilation or endoureterotomy may be considered for short, low-grade strictures, but open reconstruction is associated with higher success rates.
Nearly 60% of patients can be successfully managed with a pelvic drain and urinary decompression (nephrostomy tube, ureteral stent, and indwelling bladder catheter). Proximal, large-volume, or leaks that persist despite urinary diversion, require open repair [14].
Surgical treatment: Surgical management includes drainage of urinomas, resection of devitalized ureter if needed and ureteral reimplantation. The residual ureter may be short in which case a bladder flap may be needed. In some cases a cutaneous ureterostomy with omental interposition is undertaken.
Patients, who develop transplant ureteral fistulae, can be treated endourologically [15].
Lymphocele
Another cause of high drain output after renal transplantation is a lymphocele which is a collection of lymphatic fluid around the kidney. It is a hard fibrous cavity without epithelial lining containing lymph [16].
Before ultrasound, the incidence of lymphocele ranged between 0.6 – 18% increasing to around 33% with the use of ultrasound [17,18].
The causes of lymphocele are not very well known. The disturbances in lymph flow of the transplanted kidney or the recipient secondary to dissection of lymphatics at the time of procurement or at the time of surgery respectively has been suggested as a cause for the development of lymphocele.Adult dominant polycystic kidney disease (ADPCKD) as the background disease, cellular rejection, use of mTOR inhibitors, diuretics and high dose steroids are some of the other suggested causes [19].
Lymphocele may develop between 2 weeks to 6 months post transplant surgery with most of them developing at 6 weeks. There are reports of some lymphoceles developing as late as after 3 years of transplantation [20].
Lymphoceles are mostly asymptomatic.
Diagnosis: As discussed above, the creatinine level in the fluid from lymphocele is not as high as in a urinoma and should match serum creatinine. Once it is established that the drain fluid is lymph, next question to answer is whether the lymph is recipient originated or from the transplanted kidney. CK activity, a marker of the iliac lymph, should be checked. The nomogram by Pacovsky can be used to find the contribution of renal lymph [21].
Treatment: If the lymphocele is small, it may resolve following percutaneous drainage. Bigger lymphoceles or those resistant to drainage may resolve by sclerosis with doxycycline, bleomycin, talc or fibrin glue. In some cases deroofing, either laparoscopic or open, is needed. Sclerosis may, however, cause ureteric fibrosis.
Hematoma
The hematoma can develop spontaneously, post biopsy or post surgical trauma.
The clinical presentation can be graft dysfunction as a result of hypovolemia or hydronephrosis secondary to displacement by the hematoma [22]. Clinical signs of hypovolemia may or may not be present.
Pre transplant use of anticoagulants adds to the risk of bleeding while as living donor transplant recipients and those with lower BMI carry lesser risk of bleeding [23].
The drain fluid may contain frank blood or be serosanguinous.
Hematomas are usually echogenic on US but lose echogenicity as they age. Hematomas have high-attenuated components in acute stage, but attenuation diminishes with time[22].
The hematoma can be managed conservatively if it is small but needs surgical exploration if large or compressing. There is a risk of infection and abscess formation.
Abscess
Urinoma, hematoma and other collections around a transplanted kidney can transform into an abscess. The clinical signs of sepsis may or may not be present. The drain fluid contains high number of WBCs.
Inflammatory markers may be elevated but can be so as a result of recent surgery or may be blunted because of immunosuppression.
As opposed to renal cortical abscesses, the perinephric abscesses are more likely to be due to gram negative bacteria especially Enterobacteriaceae. Rare organisms like salmonella have been reported [24].
Abscesses can have a non-specific appearance at US while as CT may differentiate them from other collections because of the gas present in an abscess [22].
Drainage would be needed in most of the cases [25,26].
Conclusion
Urinoma is not uncommon in early post transplant period and should always be in differential diagnosis of a collection around renal transplant or in recipients with high drain output. The drain fluid should be sent for biochemical assay including creatinine level and be matched with the serum creatinine. The management may be conservative or surgical depending upon the size and location of the urinary leak. Conservative management includes percutaneous drainage and should be undertaken regardless whether a surgical exploration is considered or not.
- Siedlecki A, Irish W, Brennan DC (2011) Delayed Graft Function in the Kidney Transplant. Am J Transplant 11: 2279–2296. Link: https://goo.gl/nEsvfY
- Englesbe MJ, Dubay DA, Gillespie BW, Moyer AS, Pelletier SJ, et al. (2007) Risk factors for urinary complications after renal transplantation. Am J Transplant 7: 1536-1541. Link: https://goo.gl/UdTydk
- Mah TJ, Mallon DH, Brewster O, Saeb-Parsy K, Butler AJ, et al. (2017) Ureteric complications in recipients of kidneys from donation after circulatory death donors. Clin Transplant 31: Link: https://goo.gl/PxQKYV
- Nie ZL, Zhang KQ, Li QS, Jin FS, Zhu FQ, et al. (2009) Urological complications in 1,223 kidney transplantations. Urol Int 83: 337–341. Link: https://goo.gl/DZ1hA5
- Zavos G, Pappas P, Karatzas T, Karidis NP, Bokos J, et al. (2008) Urological complications: analysis and management of 1525 consecutive renal transplantations. Transplant Proc 40: 1386–1390. Link: https://goo.gl/dd9Exq
- Hamouda M, Sharma A, Halawa A (2018) Urine Leak after Kidney Transplant: A Review of the Literature. Exp Clin Transplant 1: 90-95. Link: https://goo.gl/zqxf3d
- Flores-Gama F, Bochicchio-Riccardelli T, Mondragón-Ramírez G (2010) Determination of creatinine in drained liquid. Urinary leak or lymphocele? Cir Cir 78: 327-332. Link: https://goo.gl/DnDaAN
- Yu JQ, Zhuang H, Xiu Y, El-Haddad G, Kumar R, et al. (2005) Small Urine Leak After Renal Transplantation: Detection by Delayed 99mTc-DTPA Renography—A Case Report. J Nucl Med Technol 33: 31-33 Link: https://goo.gl/ZK9SDR
- Dirlik A, Erinç R, Özcan Z, Duman S, Özkahya M, et al. (2001) Diagnosis Of Urinary Leakage In Renal Transplant Patients: Ultrasonographic, Clinical And Scintigraphic Findings. Official Journal of the Turkish Society of Nephrology 10: 239-243. Link: https://goo.gl/jnZ3hM
- Son H, Heiba S, Kostakoglu L, Machac J (2010) Extraperitoneal urine leak after renal transplantation: the role of radionuclide imaging and the value of accompanying SPECT/CT - a case report. BMC Med Imaging 10: 23. Link: https://goo.gl/9GcomL
- Benoit G, Blanchet P, Eschwege P, Alexandre L, Bensadoun H, et al. (1996) Insertion of a double pigtail ureteral stent for the prevention of urological complications in renal transplantation: a prospective randomized study. J Urol 156: 881-884. Link: https://goo.gl/89cPkU
- Dominguez J, Clase CM, Mahalati K, MacDonald AS, McAlister VC, et al. (2000) Is routine ureteric stenting needed in kidney transplantation? A randomized trial. Transplantation 70: 597-601. Link: https://goo.gl/hytXBt
- Matalon TA, Thompson MJ, Patel SK, Ramos MV, Jensik SC, et al. (1990) Percutaneous Treatment of Urine Leaks in Renal Transplantation Patients. Radiology.174: 1049-1051. Link: https://goo.gl/WEGrAe
- Duty BD, Barry JM (2015) Diagnosis and management of ureteral complications following renal transplantation. Asian Journal of Urology 2: 202-207. Link: https://goo.gl/U14AmD
- Alcaraz A, Bujons A, Pascual X, Juaneda B, Martí J, et al. (2005) Percutaneous Management of Transplant Ureteral Fistulae Is Feasible in Selected Cases. Villavicencio. Transplant Proc 37: 2111-2114. Link: https://goo.gl/gM94F3
- Lima ML, Cotrim CA, Moro JC, Miyaoka R, D'Ancona CA, et al. (2012) Laparoscopic treatment of lymphoceles after renal transplantation. Int Braz J Urol 38: 215–221. Link: https://goo.gl/r37Bua
- Howard RJ, Simmons RL, Najarian JS (1976) Prevention of lymphoceles following renal transplantation. Ann Surg 184: 166–168. Link: https://goo.gl/5uwyu1
- Dubeaux VT, Oliveira RM, Moura VJ, Pereira JM, Henriques FP (2004) Assessment of lymphocele incidence following 450 renal transplantations. Int Braz J Urol30: 18–21 Link: https://goo.gl/P9tvsL
- Zietek Z, Sulikowski T, Tejchman K, Sieńko J, Janeczek M, et al. (2007) Lymphocele after kidney transplantation. Transplant Proc 39: 2744–2747 Link: https://goo.gl/rvcEMQ
- Ranghino A, Segoloni GP, Lasaponara F, Biancone L (2015) Lymphatic disorders after renal transplantation: new insights for an old complication. Clinical Kidney Journal 8: 615–622. Link: https://goo.gl/YBDLe7
- Pacovsky J, Hyspler R, Navratil P, Brodak M (2010) The estimation of posttransplant lymphocele origin using creatine kinase activity. Ups J Med Sci 115: 187–192. Link: https://goo.gl/k2WjcZ
- Akbar SA, Jafri SZ, Amendola MA, Madrazo BL, Salem R, et al. (2005) Complications of Renal Transplantation. Radiographics 25: 1335-1356. Link: https://goo.gl/cm3mK9
- Hachem LD, Ghanekar A1,2, Selzner M1,2, Famure O1,3, Li Y, et al. (2017) Postoperative surgical‐site hemorrhage after kidney transplantation: incidence, risk factors, and outcomes. Transpl Int 30: 474-483. Link: https://goo.gl/F17as5
- Catoe H, Ramdial J, Dejman A, Kupin W (2017) Salmonella Abscess in a Failed Transplanted Kidney. J Infect Non-Infect Dis 3: 019. Link: https://goo.gl/Mvf4gT
- Coelho RF, Schneider-Monteiro ED, Mesquita JL (2007) Renal and perinephric abscesses: analysis of 65 consecutive cases. World J Surg 31: 431-436. Link: https://goo.gl/UYBXMw
- Saiki J, Vaziri ND, Barton C (1982) Perinephric and Intranephric Abscesses: A Review of the Literature. West J Med 136: 95–102. Link: https://goo.gl/zJHMzw
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
