Annals of Pancreatic Disorders and Treatment
Alcohol Consumption and Pancreatitis Mortality
YE Razvodovsky*
Cite this as
Razvodovsky YE (2017) Alcohol Consumption and Pancreatitis Mortality. Ann Pancreat Disord Treatm 1(1): 007-009. DOI: 10.17352/apdt.000003Background: Pancreatitis is a major public health problem with high associated economic costs. Accumulated research and empirical evidence suggests that excessive alcohol consumption is a major risk factor for both acute and chronic pancreatitis. In line with this evidence we assume that devastating combination of higher level of alcohol consumption per capita and drinking of vodka results in a close association between binge drinking and pancreatitis mortality at the aggregate level in Russia. This paper was design to estimate the aggregate level effect of binge drinking on pancreatitis mortality rate in Russian.
Method: Trends in age-adjusted, sex-specific pancreatitis mortality and fatal alcohol poisoning rate (as a proxy for binge drinking) from 1956 to 2015 were analyzed employing a distributed lags analysis in order to ass’s bivariate relationship between the two time series.
Results: The results of the time series analysis indicates the presence of a statistically significant association between the two time series at zero lag for male (r = 0.72; S.E. = 0.13), and for female (r = 0.36; S.E. = 0.13).
Conclusion: The results of present study support the hypothesis that alcohol played a crucial role in pancreatitis mortality fluctuation in Russia over the past decades. This study also indicates that substantial proportion of pancreatitis deaths in Russia is due to acute effect of binge drinking. The findings from the present study have important implications as regards pancreatitis mortality prevention indicating that a restrictive alcohol policy can be considered as an effective measure of prevention in countries where higher rate of alcohol consumption and binge drinking pattern.
Introduction
Pancreatitis is a major public health problem with high associated economic costs [1-3]. The incidence of pancreatitis has increased in many European countries in recent decades [4,5]. Increase of acute pancreatitis over time were greater in the younger age group which probably represent an increase in alcoholic pancreatitis, as acute pancreatitis among young people is more commonly alcohol related [6]. The incidence of acute pancreatitis varies considerably throughout the region and tended to be highest in Scandinavia and Eastern Europe [5]. The reasons for geographic differences in incidence of pancreatitis are still poorly understood and most likely are because of differences in the risk factors, including alcohol consumption [7]. Since an association between alcohol abuse and pancreatitis was reported by Fried Reich [8], many studies have confirmed that excessive alcohol consumption is a major risk factor for both acute and chronic pancreatitis [9-11]. The strong support for a close link between alcohol and pancreatitis come from individual level studies [6,12]. Using dada on 17905 men and women who participated in the Copenhagen City Heart Study Kristiansen et al. [13] reported that a high alcohol intake is associated with a high risk of pancreatitis. Hazard ratios associated with drinking 1-6, 7-13, 14-20, 21-34, 35-48, and >48 drinks/week were 1.1, 1.2, 1.3, 1.3, 2.6, 3.0 respectively, compared with 0 drinks/week. A recent systematic review and meta-analysis of epidemiologic studies on alcohol consumption and pancreatitis published between 1980 and 2008 found a monotonic and approximately exponential dose-response relationship between average volume of alcohol consumption and the risk of pancreatitis [14]. The risk curve between alcohol consumption and pancreatitis was relatively flat at low levels of alcohol consumption and it increased markedly with increasing levels of consumption. Individuals consuming 36 grams of alcohol daily, had a relative risk of 1.2 (95%; CI: 1.2-1.3), compared with non-drinkers. Whereas those with a daily alcohol intake of 96 grams, had a four-fold increased risk of pancreatitis (RR=4.2; CI:3.1-5.7), relative to non-drinkers. This study also provided evidence supporting the existence of a threshold effect (about 4 drinks daily) between alcohol consumption and the risk of pancreatitis [14]. Collectively, these findings suggest that the total amount of alcohol consumed is a critical factor in producing chronic alcohol-induced pancreatic damage.
There is, however, evidence that pattern of drinking and beverage preference may have modifying influence on pancreatitis risk independently of the amount of alcohol consumed. A follow-up study from Sweden revealed a dose-response association between the amount of spirits consumed on a single occasion and the risk of acute pancreatitis [15]. After multivariate adjustments, there was a 52% (95%; CI: 1.1-2.1) increased risk of acute pancreatitis for every increment of five standard drinks of spirits consumed on a single occasion. At the same time, there was no association between frequency of alcohol consumption and total monthly alcohol consumed on the risk of acute pancreatitis [15]. There is also empirical evidence suggesting that the holidays binge drinking may influence on the incidence of acute pancreatitis. In particular, Roberts et al. [16] reported an increased admission rate for alcoholic acute pancreatitis during the Christmas and New Year period, when there is a peak in the consumption of alcohol.
Furthermore, Nakamura et al. [17] reported that higher risk for chronic pancreatitis in alcohol-dependent men was associated with drinking spirits rather than lower-alcohol beverages. In contrast, Gerloft et al. [18] found that beer dose-dependently increases basal amylase secretion of rat pancreatic acinal cells, while wine and hard liquor had no effect on amylase secretion neither diluted to the ethanol concentration of beer nor undiluted. It seems that the risk of alcohol-induced pancreatitis differs by beverage type, such that particularly spirits, but also beer consumption has stronger effects than does wine drinking.
Although the association between alcohol and pancreatitis has been well documented, the precise magnitude of the impact of alcohol remains poorly quantified. At the individual level, the proportion of cases of pancreatitis attributed to alcohol varies widely among countries and range from 50 to 90% [9,11]. With respect to population drinking and mortality from pancreatitis, the evidence is fairly limited. The only prior study applying the ARIMA time-series analysis found a positive relationship between alcohol consumption measured by alcohol sales and pancreatitis mortality in 14 western European countries [7]. According the poled estimates for northern, mid- and southern Europe, the strongest effect was found in northern Europe. The results from this study suggest that an increase in per capita alcohol consumption of 1 litres is followed by an increase in pancreatitis mortality of 5-15% in most countries, but by a 30-40% in Sweden and Norway. In most countries, the proportions of alcohol-attributable mortality from pancreatitis fall within the range between 40 and 80% [7]. It appears that the effect of alcohol on pancreatitis mortality rate was stronger in the northern European spirits countries characterized by a binge drinking pattern, than in the southern European wine countries with a high average consumption, which is more evenly distributed throughout the week [7].
Russia ranks among the world’s heaviest drinking countries with an annual sales rate about 10 litres of pure alcohol per capita [19]. There is common believe that high level of alcohol consumption in conjunction with binge drinking pattern is a major determinant of high alcohol-related mortality rates in Russia [20-24]. Furthermore, the most recent estimates suggest that 63.1% of all male pancreatitis deaths and 26.8% female deaths in Russia could be attributed to alcohol [25].
The aim of the present study was to estimate effect of binge drinking on pancreatitis mortality rate in Russian using aggregate-level data of pancreatitis mortality and fatal alcohol poisoning rates (as a proxy for binge drinking).
Methods
Data
The data on sex-specific pancreatitis and alcohol poisoning mortality rates per 1000.000 of the population are taken from the Russian vital statistic. The cause of death classification in Russia has undergone several changes during the last decades. Until 1999, the Russian vital statistics registration system used the Soviet coding scheme to classify cause of death. From 1999 a new coding system based on the International Classification of Diseases (ICD)-10 was introduced and it has been claimed that the Russian system of coding is compatible with ICD-10 codes K 85 (acute pancreatitis) – K 86.0/86.1 (chronic pancreatitis).
It should be noted that in Russia the fatal alcohol poisoning rate is likely to be a good measure of heavy episodic drinking [23]. Therefore, a common approach is to use the fatal alcohol poisoning rate as an indicator of binge drinking in this country.
Statistical analysis
The statistical analysis was performed using the package “Statistica”. It is generally agreed that bivariate correlations between the two raw time-series are spurious due to common sources of trends and autocorrelation [26]. Therefore in order to reduce the risk of obtaining a spurious relation between two variables that have common trends, the trends should be removed by means of a differencing procedure: ∇xt = xt - xt-1 This means analyzing annual changes rather than raw data. The process of removing systematic variation within time series prior to the examination of potential causal relationships is referred to as “prewhitening” [27]. A further step entails the inspection of the cross-correlation function in order to estimate the association between the two prewhitened time series. We used an unconstrained polynomial distributed lags analysis to estimate the relationship between the time series fatal alcohol poisoning (independent variable) and pancreatitis mortality (dependent variable) in this paper.
Results
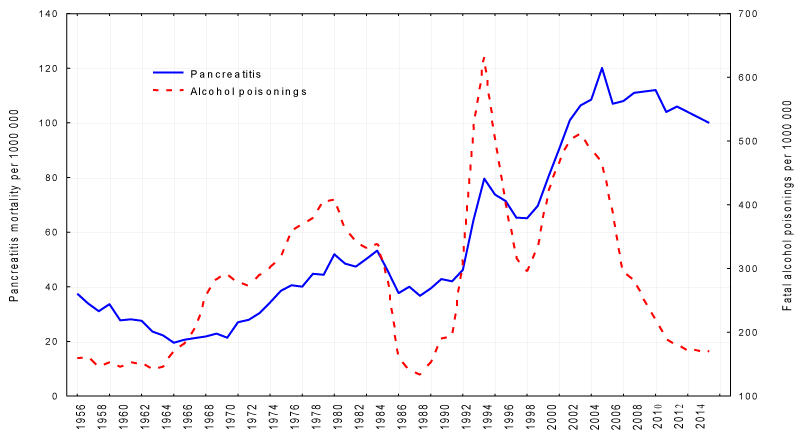
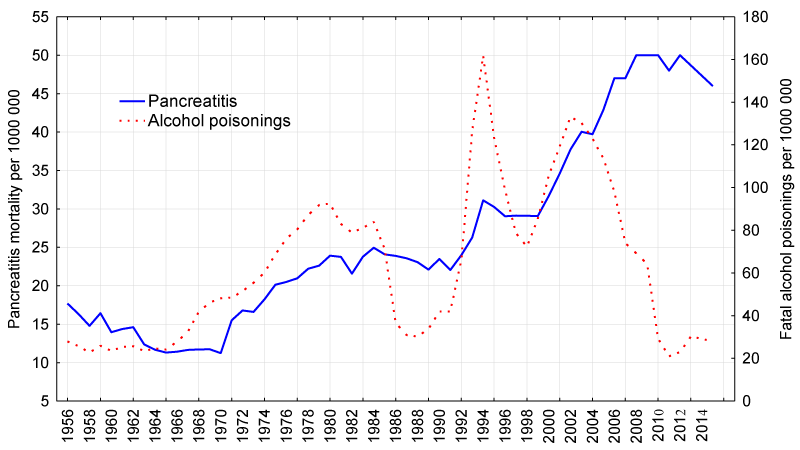
The trends in the age-adjusted, sex-specific pancreatitis mortality rates are displayed in Figures 1,2. For both sexes the time series pancreatitis mortality rates fluctuated greatly over the period: rose steadily between 1965 and 1980; decreased markedly between 1984-1986 (by 29.3% and 5.6% for men and women respectively), than started on an upward trend from 1988-1989, before increasing substantially during 1992 to 1994 (by 72.3% and 29.6% for men and women respectively). From 1995-1998 there was a fall in the rates before they again jumping dramatically between 1998 and 2005/2008 (by 84.3% and 71.8% for men and women respectively) and then started to decrease in the most recent years. Although the trends in pancreatitis mortality rates are rather similar over time series for both sexes, the male pancreatitis mortality rate tends to fluctuated across time series to a much greater extent than the female rate.
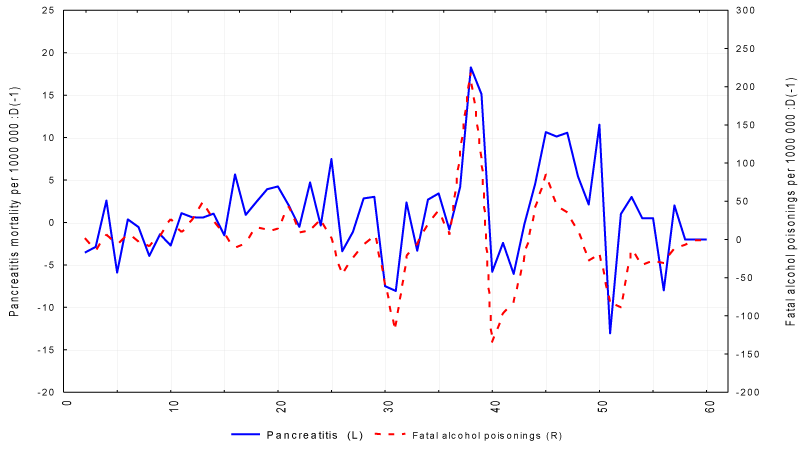
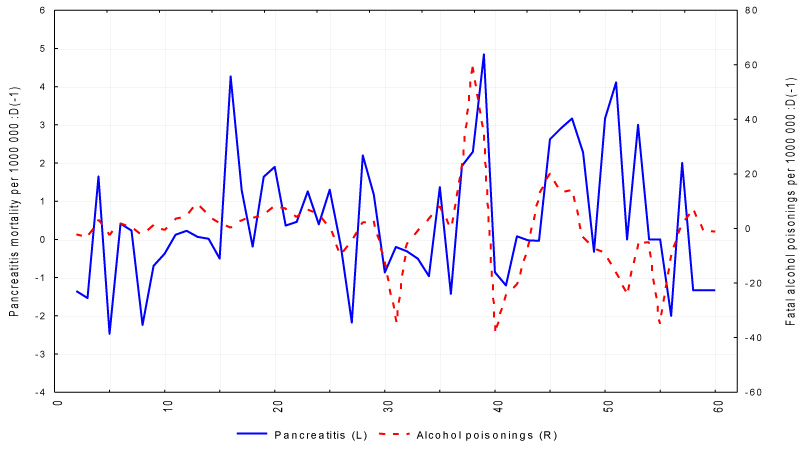
The graphical evidence suggests that the trends in both alcohol poisoning and pancreatitis mortality for males and females seem to follow each other across the time-series (Figures 1,2). The Spearman’s correlation analysis suggests a strong positive association between the two variables for male (r=0.59; p=0.000) and female (r=0.51; p=0.000). As can be seen from figures 1,2 there are linear and S-shape trends in the time series. These trends were removed by means of first-order differencing procedure (Figures 3,4). After pre-whitening the cross-correlations between fatal alcohol poisoning and pancreatitis mortality time series were inspected. The outcome indicated statistically significant cross-correlation between the two variables for male (r = 0.72; SE = 0.13) and female (r = 0.36; SE = 0.13) at zero lag. The results of the distributed lags analysis also suggest that only contemporaneous correlation (lag 0) is statistically significant for both males and females (Tables 1,2).
Discussion
The time series analysis suggests a fairly quick response of pancreatitis mortality rates to changes in population binge drinking. The instantaneous response in mortality rates from chronic alcohol-related diseases seem quite surprising when considering the long latency period at the individual level. There is, however, a reasonable explanation for this seeming inconsistency. It is well recognized, that pancreatitis mortality is the classical indicator of harmful effect of chronic heavy drinking (chronic pancreatitis) and also associated with episodic heavy drinking (acute pancreatitis), thus reflecting the acute and chronic consequences of binge drinking [11]. Therefore, the contemporaneous association between the two variables may support the point that binge drinking is an important determinant of pancreatitis mortality in Russia.
Additional support for the hypothesis that unfavorable mixture of higher overall level of alcohol consumption and binge drinking of spirits is a major risk factor for pancreatitis mortality in Russia provides the results of time-series analysis focused on the relation between the sale of different alcoholic beverages and pancreatitis mortality rates. It was reported that vodka consumption as measured by sale was significantly associated with both male and female pancreatitis rate: 1 litre changes in per capita vodka sale was associated with increase in pancreatitis mortality rates by 10.3% for men and by 3.2% for women [28].
It should be emphasized, that the size of the bivariate association between binge drinking and pancreatitis deaths for men is substantially greater than for women. The harmful drinking pattern might be responsible for these gender differences. The population surveys from Russia show consistently higher rates of binge drinking among men than women [29].
Understanding the reasons the substantial fluctuations in pancreatitis mortality rate in Russia over recent decades is very important from a public health perspective. There is evidence that the fatal alcohol poisoning and pancreatitis mortality trends in Russia influenced by the three major factors: Gorbachev’s anti-alcohol campaign 1985-88; severe socioeconomic crisis imposed by rapid societal transformation in the early 1990s; financial crisis and worsening economic situation in 1998; the period of economic growth over the last decade.
The Gorbachev’s anti-alcohol campaign (1985-1988) was unprecedented in scale and it consisted of several broad measures designed to limit the availability and affordability of alcohol [21]. A fairly close match between trends in fatal alcohol poisoning and pancreatitis mortality during the Gorbachev’s anti-alcohol campaign may be used as evidence for the hypothesis suggesting that alcohol is responsible for a substantial number of pancreatitis deaths in Russia. This empirical evidence also indicates that a restrictive alcohol policy can be considered as an effective measure of pancreatitis mortality prevention.
The underlying cause of the alcohol-related mortality crisis in Russia during transition has been hotly debated, but still remains poorly understood [19, 21]. This crisis could be the combined result of lagged “catch-up” mortality (the lagged effects of the anti-alcohol campaign) and the increase in the availability and affordability of alcohol [30]. It seems plausible that alcohol is a key variable in explaining the increase in the pancreatitis mortality rate in the early-1990s. An increase of alcohol consumption in this period was to a great extent due to increase of alcohol availability following the repeal of the state alcohol monopoly in January 1992 [21].
There are several potential factors behind the decrease in alcohol consumption and pancreatitis mortality rate between 1994 and 1998. They include better regulation of the alcohol market that may have resulted in a relative increase in prices for vodka compared to those for food products [21]. Another possible factor in the decrease in alcohol consumption was impoverishment and decrease in the purchasing capacity of the population due to unpaid or delayed salaries [30]. The subsequent rise in fatal alcohol poisonings and pancreatitis mortality rates from 1998 may be associated with the financial crisis which resulted in the relative fall in price for vodka [21].
Before concluding, several potential limitations of this study must be mentioned. In particular, a close relationship between fatal alcohol poisonings and pancreatitis mortality does not rule out the possibility that other factors have also influenced the development pancreatitis mortality rate. Although alcohol is regarded as the most important risk factor for pancreatitis, a number of other causal factors that influence the risk of development of pancreatitis have been identified, including diet and smoking [10]. The presence of these causal factors is likely to have distorted the estimated alcohol effects. It seems that the role of non-alcohol causes in pancreatitis mortality increased during the last decade.
Further, surrogate alcohols cannot be avoided when discussing the association between alcohol consumption and a risk for the development of alcoholic pancreatitis. The initial evidence of the involvement of surrogate alcohols in the pathogenesis of pancreatitis came from Goa (India), where the patients admitted with an acute attack of pancreatitis was more likely to have consumed country-made alcohol rather than the licensed beverages [31]. This empirical evidence prompted the analytical study, which showed that locally distilled alcoholic beverages, regularly consumed by patients developing alcoholic pancreatitis contained a higher level of compounds in addition to ethanol including long-chain alcohols, aldehydes, acids and even traces of methanol [31]. According to “critical mass” hypothesis the presence of additional compounds in alcohol could potentiate the oxidative stress induced by ethanol and could lower the threshold for developing acute pancreatitis [32].
In Russia, the consumption of homemade spirits (samogon) and surrogate alcohols, also referred unrecorded alcohol, is somewhat common [33-35]. According to WHO statistics [35], unrecorded alcohol accounts for one-third of all consumption in Russia, while some estimates show a figure as high as 50% [19]. Among the most common surrogates are industrial spirits, antiseptics, lighter fluid, and medications containing alcohol [33]. It also seems very likely that illegally distilled, counterfeit, and surrogate alcohol poses a risk to human health, playing an important role in the high level of alcohol-related deaths in Russia. It was found that home-made spirits contained the toxic by-products that could cause damage to the liver [33]. The findings from Izhevsk (Russia) study indicated that among working-age males who reported surrogate use, the relative risk of dying from causes directly related to problem drinking (e.g., alcoholic psychosis, alcoholic cardiomyopathy, alcoholic liver cirrhosis, and acute alcohol poisoning) was 25.5 in relation to those who consumed only legal alcoholic beverages [36]. Surrogates consumption increased markedly in Russia following the abolishment of the state alcohol monopoly in January 1992 [33].
Several researchers argue that increase in surrogates consumption is one of the most important predictor of the dramatic grows in pancreatitis mortality in the early 1990s [21]. A similar rapid rise in consumption of illicitly produced alcohol and surrogates has occurred in 2006, when amendments were introduced to the Federal Law “On State Regulation of the Production of Ethyl Alcohol, Alcohol and Alcohol-Containing Products”, which seriously impacted the alcohol situation in the country [37]. Under the conditions of excessive demand, the lack of licensed alcohol provoked an epidemic of poisonings by surrogates (industrial fluid, antiseptics, and household chemicals) [37].
In conclusion, the results of present study suggest a positive relation between fatal alcohol poisoning and pancreatitis mortality rates at aggregate level and support the hypothesis that alcohol played a crucial role in pancreatitis mortality fluctuation in Russia over the past decades. This study also indicates that substantial proportions of pancreatitis deaths in Russia are due to acute effect of binge drinking. The findings from the present study have important implications as regards pancreatitis mortality prevention indicating that a restrictive alcohol policy can be considered as an effective measure of prevention in countries where higher rate of alcohol consumption and binge drinking pattern.
- Liao KF, Cheng KC, Lin CL, Lai SW (2017) Etodolac and the risk of acute pancreatitis. BioMedicine-Taiwan.7: 25-9. Link: https://goo.gl/AnNeur
- Liao KF, Lin CL, Lai SW, Chen WC (2016) Sitagliptin use and risk of acute pancreatitis in type 2 diabetes mellitus: A population-based case-control study in Taiwan. Eur J Intern Med.27: 76-9. Link: https://goo.gl/c7W0wa
- Banks PA (2002) Epidemiology, natural history, and predictors of disease outcome in acute and chronic pancreatitis. Gastrointestinal Endoscopy.56: 226–230. Link: https://goo.gl/CPd71L
- Yadav D, Lowenfels AB (2006) Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas.33: 323-330. Link: https://goo.gl/lAOU0P
- Yadav D (2011) Recent advances in the epidemiology of alcoholic pancreatitis. Current Gastroenterologic Repoprts.13: 157-165. Link: https://goo.gl/1uTk9M
- Roberts SE, Williams JG, Meddings D, Goldacre MJ (2008) Incidence and case fatality for acute pancreatitis in England: geographical variation, social deprivation, alcohol consumption and etiology-a record linkage study. Alimentary Pharmacology & Therapeutics. 28: 931-941. Link: https://goo.gl/NxfmJO
- Ramstedt M (2004) Alcohol and pancreatitis mortality at the population level: experiences from 14 western countries. Addiction.99: 1255–1261. Link: https://goo.gl/3O31pB
- Friedreich N (1878) Diseases of the pancreas. In: Cyclopedia of the Practice of Medicine. Ed. H. Ziemssen. Sampson Low, London. Vol. 8. p. 551.
- Gullo L (2005) Alcohol and chronic pancreatitis: leading or secondary etiopathogenic role? Journal of the Pancreas.6: 68–72. Link: https://goo.gl/rwivgU
- Cote GA, Yadav D, Slivka A, Anderson MA, Burton FR. et al. (2011) Alcohol and smoking as risk factors in an epidemiology study of patients with chronic pancreatitis. Clinical Gastroenterology and Hepatology.9: 266–273. Link: https://goo.gl/q4Rbe2
- Bujanda L (2013) Alcohol consumption on pancreatic diseases. World Journal of Gastroenterelogy.9: 638–647. Link: https://goo.gl/cLA5i2
- Pelli H, Lappalainen-Lehto R, Piironen A, Sand J, Nordback I (2008) Risk factors for recurrent acute alcohol-associated pancreatitis: a prospective analysis. Scandinavian Journal of Gastroenterology. 43: 614-621.Link: https://goo.gl/cCRKFv
- Kristiansen L, Grønbæk M, Becker U, Tolstrup JS (2008) Risk of Pancreatitis According to Alcohol Drinking Habits: A Population-based Cohort Study. American Journal of Epidemiology.168: 932–937. Link: https://goo.gl/5fWGy3
- Irving HM, Samokhvalov AV, Rehm J (2012) Alcohol as a risk factor for pancreatitis: a systematic review and meta-analysis. Journal of the Pancreas.10: 387–392. Link: https://goo.gl/njDwkU
- Azodi OS, Orsini N, Andrén-Sandberg A (2011) Effect of type of alcoholic beverage in causing acute pancreatitis. British Journal of Surgery.98: 1609–1616. Link: https://goo.gl/jNtQ3q
- Roberts SE, Akbari A, Thorne K, Atkinson M, Evans PA (2013) The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Alimentary Pharmacology and therapeutics. 38: 539-548 Link: https://goo.gl/5jVyIX
- NakamuraY, Ishikawa A, Sekiguchi S, Kuroda M, Imazeki H, Higuchi S (2003) Spirits and gastroectomy increase risk for chronic pancreatitis in Japanese male alcoholics. Pancreas.26: 27-31. Link: https://goo.gl/py3yj5
- Gerloft A, Singer MV, Feick P (2009) Alcoholism Clinical and Experimental Research.33: 1545-1554.
- Nemtsov AV (2000) Estimates of total alcohol consumption in Russia, 1980-1994. Drug and Alcohol Dependence.58:133–142. Link: https://goo.gl/U4GkWB
- Razvodovsky YE (2002) Asociacion entre consumo de vodka y tasa de mortalidad relacionada con el alcohol, a nivel agregado, utilizando series temporales. Adicciones. 14: 497-502. Link: https://goo.gl/fQXlVy
- Nemtsov AV, Razvodovsky YE (2008) Alcohol situation in Russia, 1980-2005. Social and Clinical Psychiatry.2: 52–60. Link: https://goo.gl/zKmCiz
- Razvodovsky YE (2012) Estimation of alcohol attributable fraction of mortality in Russia. Adicciones. 24: 1–7. Link: https://goo.gl/c5NCUW
- Stickley A, Leinsalu M, Andreew E, Razvodovsky YE, Vagero D, McKee M (2007) Alcohol poisoning in Russia and the countries in the European part of the former Soviet Union, 1970-2002. European Journal of Public Health.17: 444–449. Link: https://goo.gl/EOTczc
- Stickley A, Razvodovsky Y, McKee M (2009) Alcohol and mortality in Russia: A historical perspective. Public Health.123: 20-26. Link: https://goo.gl/W6c9Sv
- Razvodovsky YE (2014) Alcohol consumption and pancreatitis mortality in Russia. Journal of the Pancreas 15: 214-219. Link: https://goo.gl/acuXBU
- Norström T, Skog OJ (2001) Alcohol and mortality: methodological and analytical issue in aggregate analysis. Addiction. 96: 5–17. Link: https://goo.gl/HTqaGX
- Box GEP, Jenkins GM (1976) Time Series Analysis: forecasting and control. London. Holden-Day Inc.
- Razvodovsky YE (2015) The effect of beverage type on pancreatitis mortality in Russia. Pancreas. 44: 832-833. Link: https://goo.gl/fbRp5D
- Nilssen O, Averina M, Brenn T, Drox J, Kalinin A, et al (2005) Alcohol consumption and its relation to risk factors for cardiovascular disease in the north-west of Russia: the Archangelsk study. International Journal of Epidemiology. 34:781–88. Link: https://goo.gl/KTbtIk
- Nemtsov AV, Davydov KE, Razvodovsky YE (2009) Comparative analysis of the alcohol situation in Belarus and Russia. Narcologia. 1:52–60. Link: https://goo.gl/rzCHH3
- Barreto SG, Rodrigues J (2008) Acute pancreatitis in Goa - a hospital-based study. J Indian Med Assoc. 106: 575-578. Link: https://goo.gl/mEc77J
- Barreto SG, Saccone GT (2010) Alcohol-induced acute pancreatitis: the 'critical mass' concept. Med Hypotheses. 75: 73-76. Link: https://goo.gl/O2A4Bz
- Razvodovsky YE (2008) Noncommercial alcohol in central and eastern Europe, ICAP Review 3. In: International Center for Alcohol Policies, ed. Noncommercial alcohol in three regions. Washington. Link: https://goo.gl/o9Uyc1
- Razvodovsky YE (2013) Estimation of the level of alcohol consumption in Russia. ICAP Periodic Review on Drinking and Culture. Issue 8. b:7–10. Link: https://goo.gl/85n4lM
- World Health Organization, Global Status Report on Alcohol and Health, World Health Organization, Geneva, Switzerland, 2014. Link: https://goo.gl/eBnXS0
- Leon DA, Saburova L, Tomkins S, Andreev E, Kiryanov N et al (2007) Hazardous alcohol drinking and premature mortality in Russia: a population based case-control study. Lancet. 369: 2001-2009. Link: https://goo.gl/5oshDU
- Nemtsov AV, Razvodovsky YE (2016) Russian alcohol policy in false mirror. Alcohol & Alcoholism. 51: 626-627. Link: https://goo.gl/Fpz3Zx
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
