International Journal of Oral and Craniofacial Science
Maxillary protraction with bimaxillary bone anchor and mini rigid surgical fixation plates in patient with Bilateral Cleft Lip and Palate Sequelae: Case report
Acosta Rangel Monica C1*, Ayuso Arce América2, Amador Jiménez Olaf3
2Orthodontist, Professor at the Technological University of Mexico, Mexico
3Oral and Maxillofacial Surgeon, Maxillofacial Surgeon Military School of Health Graduates of the University of the Army and Mexican Air Force, Mexico City, Mexico
Cite this as
Acosta Rangel M, Ayuso Arce A, Amador Jimenez O(2018) Maxillary protraction with bimaxillary bone anchor and mini rigid surgical fixation plates in patient with Bilateral Cleft Lip and Palate Sequelae: Case report. Int J Oral Craniofac Sci 4(1): 005-009. DOI: 10.17352/2455-4634.000035The objective is to evaluate the effects of maxillary protraction by means of a bimaxillary bone anchorage as well as its progress by fixing mini plates in patients with Bilateral Cleft Lip and Palate Sequela, based on the protocol of Clerck and Cha et al. HGO CM La Raza and the Technological University of Mexico UNITEC.
Introduction
One of the sequels due to the surgical repair of the Cleft Lip and Palate (LPH) [1], is the retrusion of the middle facial third, affecting the three-dimensional growth of the maxilla. The contracture due to scar tissue is one of the most important causes of maxillary growth alterations [2], reporting an incidence of 15% to 25% in most series [3]. The main clinical features such as concave profile, anteroposterior deficiency of the paranasal and zygomatic region, excessive buccal corridors, negative horizontal bite, anterior crossbite produce functional alterations in the masticatory system and dysarthria causing nasopharyngeal constriction as well as damaging the physical appearance of the expensive.
The severity of maxillary hypoplasia results from factors such as: the number of surgeries performed or the not early orthopedic maxillary intervention [4,5]. Subsequently treatment in these sequelae depends mainly on the degree of involvement as well as the age of the patient. This group of patients represents a challenge in the treatment due to the skeletal deformity, usually greater than in dentofacial deformities not associated with LPH [6-8].
Different alternatives for the treatment of maxillary hypoplasias, among those reported in the literature (Table 1) [9], we have Delaire that uses orthopedic protraction with facial mask and maxillary splint for a dental anchor; Molina [10], pioneer in maxillary distraction, makes use of an orthopedic mask and elastic traction [11]; subsequently the establishment of an external distractor which is still in use. Recently, maxillary protraction with bimaxillary bone anchorage has been described, without performing corticotomies, in reports of case series [12-14], so it is imperative to analyze the particular variables in each patient, as well as to know indications and limitations of each technique to achieve optimal and stable results for the patient through time.
The maxilla is fully developed by intramembranous ossification, with all the growth mechanisms such as sutural connective tissue proliferation, surface apposition, resorption, translation and growth in V. The growth vector of the naso-maxilla complex is due to the oblique and parallel position of the circummaxillary sutures [17,18], which cause posterior apposition in the primary displacement in the anterior and inferior direction and in a secondary displacement by pressures of the expansion of frontal lobes; due to the pressure of the cartilage of the anterior part of the cranial base, nasal capsule and septal cartilage [19].
The greatest cross-sectional growth is completed at approximately 12 years (40% due to the divergent vertical growth of the alveolar process, the rest due to apposition in the middle palatal suture), the greater anterior anteroposterior growth is completed at the age of 14 years and the growth vertical of 16 to 20 years (sutural growth between frontal and zygomatic bones) [20,21].
Traditionally, maxillary traction has been reported with anchoring to orthopedic dental fixation devices as treatment to patients with a tendency to class III, associated with mild maxillary hypoplasias. In patients with moderate to severe skeletal discrepancies, it is contraindicated to use dental fixation related to adverse dental effects [15,16]. Performing bone anchorage allows a true movement of the maxilla, applying force directly to the maxillary complex without involving dental movements.
The advance of the maxilla by a forward movement induced by external traction forces is achieved by remodeling the circummaxillary sutures and maxillary tuberosity, stimulating the growth of the maxillary complex as soon as possible is more effective because of the greater degree of cellular activity in the maxilla [22]. The circummaxillary sutures. Kyung Suk Cha found a greater peak in the effect to external forces of protraction in one group of patients with prepubertal and pubertal growth [23], effect that decreases in the group of post puberal growth increasing the adverse dental effects, for that reason it is suggested to classify the groups of growth using carpal radiographs using the Fishman method [24].
The maxillary bone anchorage has been described with the zygomatic abutments of the maxilla or naso-maxilla, it was decided by the maxillary zygomatic due to offer sufficient bone thickness and adequate quality, ensuring stability in the anchorage before the traction forces, in addition to locating the area near the center of resistance of the maxillary complex favoring the growth vector [25].
Material and Procedure
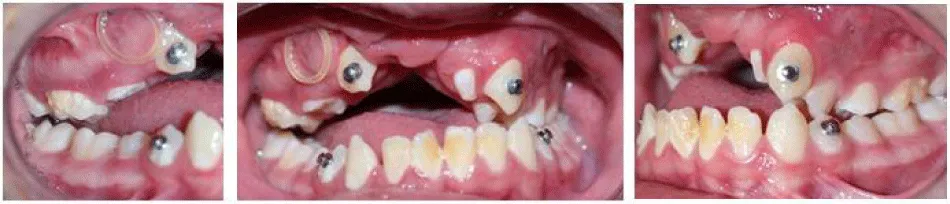
A 10-year-old male patient with Complete Bilateral Lip and Palate Sequela submitted to the protocol of Cha et al and Clerck; maxillary support with mini fixed plates and microscrews is selected, tensioning the facial mask plus the rapid expansion intra oral device with inter occlusal acrylic to open the canine class III bite and molar mixed dentition (Photograph A). The rapid expansion was repeated in four monthly periods, the first 4 days of the month, the activation was 1mm per day with simultaneous use of the protraction mask (Photograph B). Prospective observational study conducted at UNITEC and HGO CMN La Raza.
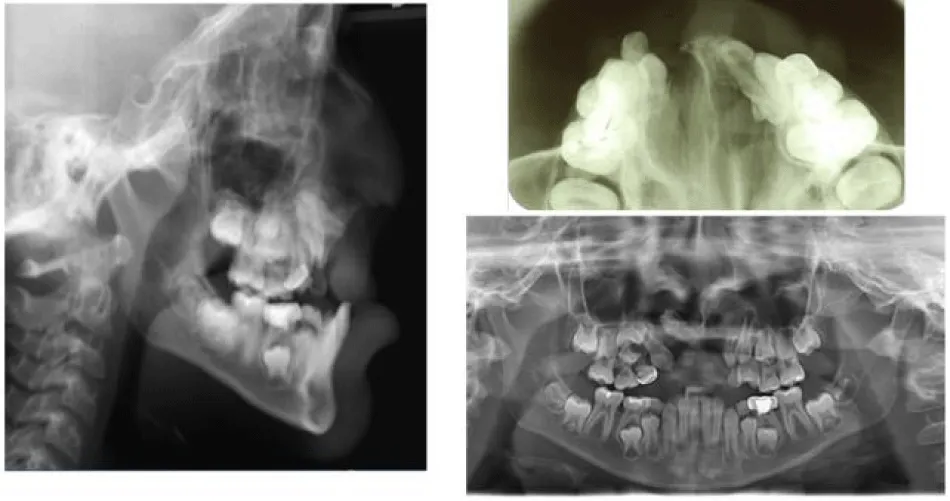
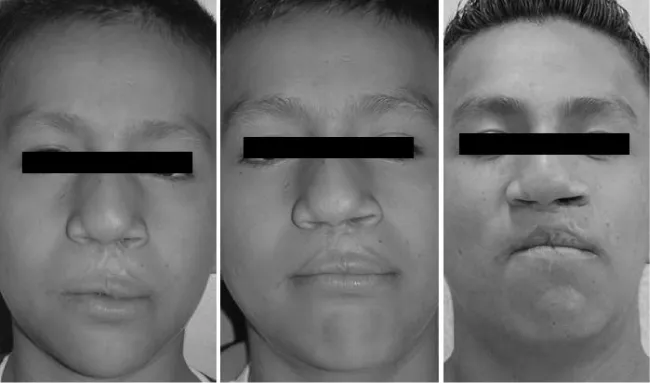
The clinical features presented by the patient were maxillary hypoplasia as a consequence of the sequelae of Bilateral Lip and Cleft Palate with anterior crossbite and convex profile, erupted lower permanent canines; the patient, according to Lamparski, was in a stage of prepubertal maturation in cervical vertebrae CS5, (Photograph C). Lateral skull radiography was taken at the beginning, clinical photography and gypsum study models. Placing two miniplates fixed with one self-drilling titanium microtubules in each infracygomatic zone. The flaps were sutured freeing the mucogingival junction, taking two weeks to recover the tissues before starting with traction, having an evaluation control with lateral x-ray of the skull, orthopantomography and pre-operative occlusal, before the placement of the miniplates and postoperative, after the placement of miniplates (Photograph D).
The activation with the elastics started in the fourth week after the procedure. Starting with one of 150gr per side, increasing to 200gr after one month; 250gr after two months to reach 600 gr per side. The force was measured with a Dontrix calibrator from the Dentaurum brand. The elastics are changed by new ones daily at night. The use of the leagues is for 24 hours a day, it is indicated to remove them for feeding, and the protraccion was carried out in a period of 12 months (Table 2).
Clinical case
11-year-old male patient who visited the National Medical Center of La Raza in the Pediatric Maxillofacial Surgery department with diagnosis of Bilateral Cleft Lip and Palate Sequelae and lyophilized bone graft, combining it with autologous calvarial sponge graft. Retouching labial to form a vestibule, performing the conventional protraccion, without maxillary advance. With concave facial profile, skeletal class III anterior maxillary deficiency, on horizontal bite of -8 mm, it starts with one over maxillary expansion in the intermolar area according to Ton-Jakel and Pont Ancho, superior interpremolar distance: 33mm, upper intermolar distance: 51mm lower interpremolar distance: 31mm, lower intermolar distance: 49mm open bite tendency. Steiner, Ricketts cephalometric analysis, where it is obtained as a list of diagnoses (Table 3).
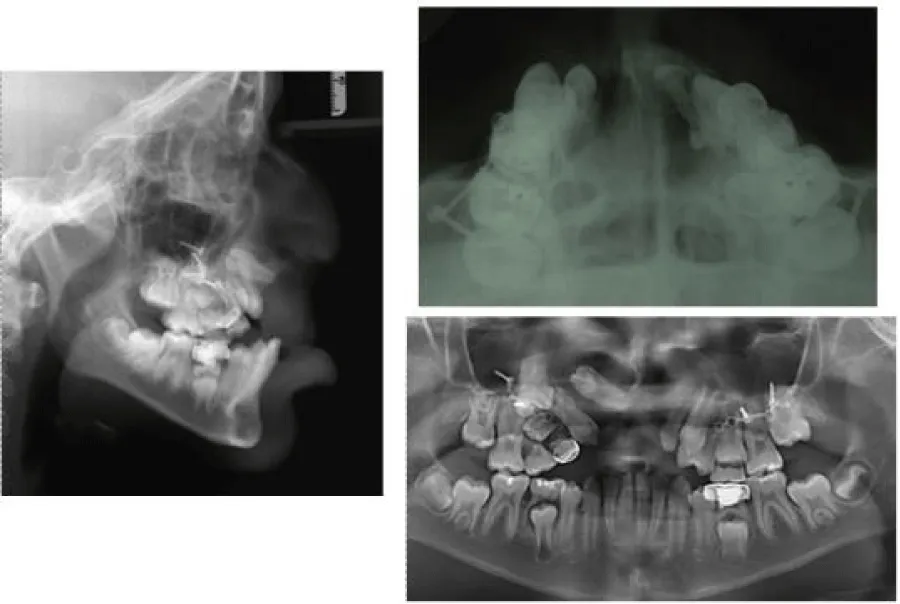
Subsequently, surgical technique was performed under general inhalation anesthesia balanced with orotracheal intubation, mucoperiosteal incision in the labial vestibule at the maxillary zygomatic buttress, raising a full thickness flap to expose the zygomatic process of the maxilla bilaterally, conformation of a 5-hole mini L-plate MODUS midface 1.5, fixing it with two monocortical screws of 1.5 mm diameter and 7 mm long, each one at the level of the basal bone in the zygomatic apophysis of the maxilla, suturing by planes with (polyglactin 910) 4-0, leaving two holes on the plate exposed at the level of inserted gingiva. After three weeks of healing, protraction forces were applied with elastics in class III, placing a protraction mask (Photograph E). Obtaining as results the advance of the maxilla with decrease of open bite.
Discussion
Moss, with the functional matrix theory, points out that bone and cartilage lack growth determination and develop in response to the intrinsic growth of the associated soft tissues. This growth is visceral and is expressed through the sutures, producing a secondary displacement of the maxilla as a consequence of the functional requirement.
The use of mini plates in the area of the infra zygomatic fissure with the placement of miniplates supported on bone tissue and an external force such as the anterior traction with the facial mask allows an important advance in the maxilla, in addition to the fixation in the jaw, as a firm support element, it contributes to this advance in patients with growth deficit of the middle facial third (Photograph F). According to Moss, the stimulated functional matrix is favored with growth as long as this stimulus exists. Using this technique, the force vector will be in the oblique direction (forward-downward) (Photograph G). Installing mini plates with a long connecting bar in the region of the infracigomática crest (with the orthopedic fixation head that approaches the level of the occlusal plane) (Photograph H) and mini plates or implants in the most anterior and superior region of the Jaw, like the canine region, the force vector can be placed in the most horizontal direction possible.
Results
Significant results of growth modification were obtained in the patient using intermaxillary elastics and devices anchored in the maxilla and mandible. Therefore, the intermaxillary elastics can produce enough traction to stimulate the bone to change and grow, therefore, we assume that the stimulation of the direction of the force vector and the activations of the intraoral mask device, can have similar growth effects in the maxilla of growing children.
Achieving class I in canines and permanent molars, the decrease of telescopic bite, stability in the pre-maxilla from the bilateral alveolar grafts and over -3 mm bite. The patient had an excellent result with a rapid expansion of the maxilla, the traction was applied in the protraction mask following the Cha BK protocol.
Conclusions
The maxillary protraction technique originally described by Clerk [26-30]. Can be an effective treatment in patients with Cleft Lip and Cleft Palate who did not have a timely prior orthopedic control; to compensate for the anteroposterior deficiency of the middle third avoiding the unwanted effects, mainly of dental movements. It is economical compared to distractor techniques, even though it does not present all the advantages achieved with this technique.
However, it is an alternative for the stimulation of growth in this type of patients, with an adequate control in terms of facial growth, in which patients have this great deficiency, allowing a stable facial condition and acceptable aesthetic.
Thanking the photographs initials of the case to Dr García-Conejo, Graduate of the Specialty of Orthodontics, UNITEC. Atte. Dr. Monica Acosta Rangel Maxillofacial Surgeon.
- Ortiz MF, Rebeil AS, Valderrama M, Cruz R (1959) Cephalometric measurements on adult patients with non-operated cleft palate. Plast Reconstr Surg Transplant Bull 24: 53-61. Link: https://goo.gl/2eeCM5
- Long RE, Semb G, Shaw WC (2000) Orthodontic treatment of the patient with complete clefts of lip, alveolus and palate: lessons of the past 60 years. Cleft Palate Craniofac J 37: 533-538. Link: https://goo.gl/gCE5mg
- Liao YF, Mars M (2005) Long-term effects of lip repair on dentofacial morphology in patients with unilateral cleft lip and palate. Cleft Palate Craniofac J 42: 526-532. Link: https://goo.gl/NTWcqW
- Velázquez JM (2012) Prevención de las malformaciones postquirúrgicas en pacientes con labio y paladar hendidos. Cir Plast 22: 57-66. Link: https://goo.gl/qaVFKM
- Ayuso A, Torres M (2012) Botón ortopédico permanente para tratamiento del colapso maxilar postquirúrgico en pacientes de uno a dos años de edad con fisura labiopalatina unilateral completa. Seguimiento a 10 años. Cir Plast 22: 50-56 Link: https://goo.gl/EKPhWZ
- Ishikawa H, Kitazawa S, Iwasaki H, Nakamura S (2000) Effects of maxillary protraction combined with chin-cap therapy in unilateral cleft lip and palate patients. Cleft Palate Craniofac J 37: 92-97. Link: https://goo.gl/tyuxwJ
- Van den Dungen GM, Ongkosuwito EM, Aartman IH, Prahl-Andersen B (2008) craniofacial morphology of Dutch patients with bilateral cleft lip and palate and noncleft controls at the age of 15 years. Cleft Palate Craniofac J 45: 661-666. Link: https://goo.gl/byQV6C
- Seung-Hank Baek, Keun-Woo Kim (2010) new treatment modality for maxillary hipoplasia in cleft patients. Angle Orthod 4: 783-791. Link: https://goo.gl/CcL2te
- Delaire J (1971) Manufacture of the "orthopedic mask". Rev Stomatol Chir Maxillofac 72: 579-582. Link: https://goo.gl/a2ExC9
- Molina F, Ortiz Monasterio (1996) Maxillary distraction: Three years of clinical experience, in Plastic Surgical Forum, vol XIX, Proceedings of the 65th Annual Meeting of the American Society of Plastic and Reconstructive Surgeons. p 54. Link: https://goo.gl/cK9gAi
- Polley JW, Figueroa A (1997) Management of severe maxillary deficiency in childhood and adolescence through distraction osteogenesis with an external, adjustable, rigid distraction device. J Craniofac Surg 8: 181. Link: https://goo.gl/GnASpH
- De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ (2009) Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg 67: 2123-2129. Link: https://goo.gl/ZUNWa6
- Cevidanes L, Baccetti T, Franchi L, McNamara JA Jr, De Clerck H (2010) Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod 80: 799-806. Link: https://goo.gl/rDFDjb
- Heymann GC, Cevidanes L, Cornelis M, De Clerck HJ, Tulloch JF (2010) Three-dimensional analysis of maxillary protraction with intermaxillary elastics to miniplates. Am J Orthod Dentofacial Orthop 137: 274-284. Link: https://goo.gl/RB5NL3
- Meneses D, Botero P (2012) Alternativas para el tratamiento de hipoplasias maxilares. Rev CES Odont 25: 64-81. Link: https://goo.gl/BLLsQb
- Major M, Wong J (2012) skeletal anchored maxillary protraction for midface deficiency in children and early adolescents with Class III malocclusion: A systematic review and meta-analysis. JWFO 1: e47-e54. Link: https://goo.gl/sCE2wP
- Jackson GW, Kokich VG, Shapiro PA (1979) Experimental and postexperimental response to anteriorly directed extraoral force in young Macaca nemestrina. Am J Orthod 75: 318-333. Link: https://goo.gl/PRtKJ8
- Kambara T (1977) Dentofacial changes produced by extraoral forward force in the Macaca irus. Am J Orthod 71: 249-276. Link: https://goo.gl/8xmCPk
- Moss ML, Salentijn L (1969) the capsular matrix. Am J Orthod 56: 474-490. Link: https://goo.gl/jJQUTV
- Mogavero FJ, Buschang P, Wolford L (1997) Orthognathic surgery effects on maxillary growth in patients with vertical maxillary exces. Am J Orthod 111: 288-296. Link: https://goo.gl/Mtmxzk
- Savara BS, Singh IJ (1968) Norms of size and annual increments of seven anatomical measures of maxilla in boys from three to sixteen years of age. Angle Orthod 38: 104-120. Link: https://goo.gl/Jvuwus
- Melsen B, Melsen F (1982) the postnatal development of palatomaxillary region studied on human autopsy material. Am J Orthod 82: 329-342. Link: https://goo.gl/4R9WFg
- Cha K (2003) Skeletal Changes of Maxillary Protraction in Patients Exhibiting Skeletal Class III Malocclusion: A Comparison of Three Skeletal Maturation Groups. Angle Orthod 73: 26-35. Link: https://goo.gl/4q2eJT
- Fishman LS (1982) Radiographic evaluation of skeletal maturation: a clinically oriented method based on hand-wrist films. Angle Orthod 52:88-112. Link: https://goo.gl/fWimy3
- Tanne K, Matsubara S, Sakuda M (1995) Location of the centre of resistance for the nasomaxillary complex studied in a three dimensional finite element model. Br J Orthod 22: 227-232. Link: https://goo.gl/VbjwKZ
- De Clerck (2011) Success rate of miniplate anchorage for bone anchored maxillary protraction. Angle Orthod 81: 1010-1013. Link: https://goo.gl/8uB1Ms
- De Clerck H, Cevidanes L, Baccetti T (2010) Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop 138: 577-581. Link: https://goo.gl/E63uEw
- De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ (2009) Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg 67: 2123-2129. Link: https://goo.gl/VFGsVb
- De Clerck H, Geerinckx V, Siciliano S (2002) the zygoma anchorage system. J Clin Orthod 36: 455-459. Link: https://goo.gl/DrpTP7
- Heymann G, De Clerck H, Tulloch C (2010) Three-dimensional analysis of maxillary protraction with intermaxillary elastics to miniplates. Am J Orthod Dentofacial Orthop 137: 274-284. Link: https://goo.gl/RgqC6z
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
