International Journal of Oral and Craniofacial Science
The effect of Gauze Dressing use on reduction of Oronasal Fistula Rates following Cleft Palate Repair
Fatma Bilgen*, Alper Ural and Mehmet Bekerecioğlu
Cite this as
Bilgen F, Ural A, Bekerecioğlu M (2019) The effect of Gauze Dressing use on reduction of Oronasal Fistula Rates following Cleft Palate Repair. Int J Oral Craniofac Sci 5(1): 001-004. DOI: 10.17352/2455-4634.000036Background: The most incident and the most persistent complication following cleft palate repair is oronasal fistula. Fistulas involving the soft palate may be corrected via excision and primary closure; however fistulas of the hard palate constitue a majör challange.
Aims: In this study, in order to reduce the rate of oronasal fistula following cleft palate surgery, we present postoperative use of palatal gauze dressing.
Patients and Methods: The patients were enrolled randomly into two groups as Group one and two. For group two patients, at the end of operation, an antibiotic pomade absorbed sterile gauze was fixed at the palate with 2/0 silk sutures, under moderate pressure in order not to interfere with flap circulation.
Results: Of the 7 fistulas in group one, 5 were located on the hard palate and 2 on the soft palate, whereas in, 2 were located on the hard and two on the soft palate. No other complications were encountered.
Conclusion: The use of an antibiotic pomade-absorbed palatal gauze, tight adherence of palatal flaps to the underlying bone is achieved. Besides, serving as a barrier, the gauze prevents infection with food remnants and irritation with foreign bodies.
Introduction
Cleft palate and lip are one of the most common congenital anomalies worldwide with the prevalence of one in 700 live births1. In its etiopathogenesis, both genetic factors and environmental teratogens play an important role. Environmental factors include maternal smoking, alcohol, anticonvulsant and retinoic acid use, while the disease depending on genetic factors can present with syndromes according to the affected area. Family history plays a central role in non-syndromic cases [1,2].
Different surgical techniques can be applied to cleft palate repair. Primary palatoplasty techniques are well-accepted techniques, including Veau-Wardill-Kilner palatoplasty, Bardach2-flap palatoplasty, von Langenbeck palatoplasty, and Furlow palatoplasty3. However, surgical complications are seen even after repairs with these reliable techniques. Oronasal fistulas are the most common complications [3,4].
Oronasal fistulas, which cause nasal air escape, speech impairment, hearing loss, and food & drink regurgitation, are clinically relevant and require re-operation. The review of the literature has shown that the rate of oronasal fistulas change between 5 and 34% requiring re-operation following palatoplasty [4].
In the repair of oronasal fistulas, the success rate decreases due to fibrosis, poor blood supply, wound contraction, and inadequate surrounding tissue, and the rate of failure in fistula repair increases up to 65%. The main causes of oronasal fistula development include poor surgical technique, tense closure, infections, and foreign body irritation [5,6].
In this study, we aimed to decrease the rate of oronasal fistula with this method such as antibiotic pomade-absorbed palatal gauze application in cleft palate surgery considering the applicability of closed dressing to prevent foreign body irritation and infection risk.
Patients And Methods
This study was approved by the the Scientific and Ethical Review Boards of Kahramanmaraş Sütçü İmam University of Medical School (10: 16-357) 2018) and a written informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Between November 2008 and March 2017, 144 patients who were operated on due to cleft palate were included in the study. This study was designed as a hospital-based retrospective clinical descriptive study. Patients were analyzed for age, gender, cleft type (Veau classification), surgical technique, postoperative fistula formation, fistula type (Pittsburg classification) and postoperative velopharyngeal function. Velopharyngeal insuffiency was assessed according to optimal speech levels. An additional laboratory test was not performed at this stage.
Antibiotic prophylaxis was not given to any patient neither preoperatively nor postoperatively. After discharging patients a liquid diet was prescribed for three weeks.
Veau classification: Veau 1, isolated soft palate cleft; Veau 2, hard palate cleft with incomplete soft palate cleft; Veau 3, unilateral lip-alveole- palate cleft; and Veau 4 describes a bilateral lip-alveolar-palate cleft [7].
Pittsburgh classification: Type 1, uvula or bifid uvula; Type 2, soft palate; Type 3, soft palate at the junction of the hard palate combination; Type 4, hard palate; Type 5, incisive foramen, primary-secondary palate junction (seen in Veau type 4 clefts); Type 6, lingual - alveolar region; and Type 7, labial - alveolar region [8].
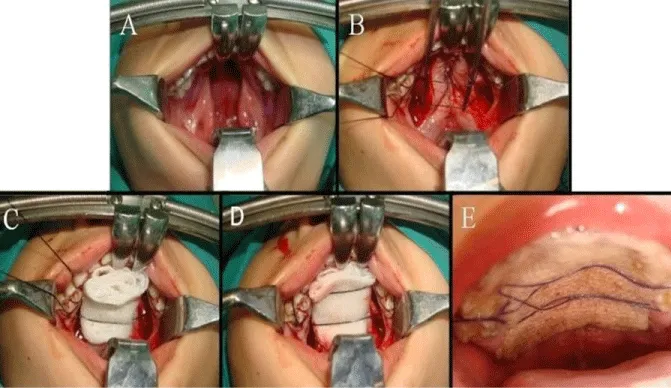
These patients were enrolled into two groups. The patients in Group 1 (n=70) were not treated with postoperative sterile gas, whereas those in Group 2 (n=74) were fixed withsterile gauze impregnated with antibiotic (bacitracin+neomycin, Thiocilline®, Abdi Ibrahim, Turkey) after surgery using moderate pressure and 2/0 silk suture to prevent flap blood circulation from any ischemia (Figure 1). The gauze was left for 3 to 5 days according to the size of the cleft. All palatal procedures were performed consecutively by a single surgeon or under his supervision within our academic teaching program.
Statistical analysis
Statistical evaluation was performed using SPSS for Windows (SPSS 10.1.3. Chicago, IL). P<0.05 was considered as significant. The Mann-Whitney U-Test wereused in relation to nonparametric and in dependentdata.
Results
A total of 144 patients with palate cleft were operated with primary palatoplasty procedures. Eighty patients (55.5%) were males and 64 (44.5%) were females. The mean age was 18 months (range: 1 to 4 years), while the mean follow-up was 25 months (range: 11 months to 3 years).
The meanage of the group 1was 19.21 ± 1.2 months and the meanage of the group 2 was 17.86 ± 0.4 months. In Group 1, there were 40 males and 30 females, in Group 2, there were 40 males and 34females.No significant difference was observed between the groups in terms of age and gender. Five of the patients were syndromic and 139 were non-syndromic. In 82 of the patients, isolated cleft palate was observed, while in 62 patients both cleft palate lip and cleft palate association was present. In Group 1, a submucous cleft was detected in 13 (18.6%), Veau Type 1 cleft in 10 (14.3%), Veau type II cleft in 15 (21.4%), Veau III cleft in 20 (28.6%), and Veau type IV cleft in 12 patients (17.1%). As the surgical technique, V-Y pushback (Veau-Wardill-Kilner palatoplasty) was performed in 80% of patients, while simple palatoplasty (Von Langenbeck) was applied to 14.3% and Furlow palatoplasty was performed in 5.7% patients in Group 1. Postoperative oronasal fistula developed in seven (10%) of the patients in Group 1. Two of the fistulas were asymptomatic, small (1-2 mm) Pittsburgh type I, while five of them were symptomatic Pittsburgh type IV with 3-6 mm. The symptomatic fistula rate was 7.14%. In addition, two of the patients with fistula had Veau Type 2, while five of them had Veau type 4.
In Group 2, submucous clefts were found in 16 (21.6%), Veau Type 1 cleft in eight (10.8%), Veau Type II cleft in 18 (24.3%), Veau Type III cleft in 16 (21.6%), Veau type IV cleft in14 (19%), and traumatic palate injuries in two patients (0.76%). As a surgical technique, 75.6%, 13.6%, and 10.8% of the patients were treated with the V-Y pushback, simple palatoplasty (Von Langenbeck), and Furlow palatoplasty, respectively. Postoperative oronasal fistulaswere observed in four (5.4%) of 74 patients in Group 2. Two of the fistulas were asymptomatic, small (1-2 mm) Pittsburgh type I, while two of them were symptomatic Pittsburgh type IV with 3-6 mm. The symptomatic fistula rate was found to be 2.7%, while two of four patients who developed oronasal fistula had Veau type 2 cleft and Veau type 4 cleft was found in four patients. There was no difference severity of the cleft between two groups. There was a significant difference in fistula rates between two groups (P<0.05) (Tables 1,2).
No velopharyngeal insufficiency was found during early and late follow-up in patients who underwent primary palatoplasty. None of the patients had major complications other than oronasal fistulas. Only one patient was re-intubated due to the development of postoperative respiratory distress. Follow-up period was uneventful.
Discussion
Cleft palate is the most common congenital craniofacial anomaly treated by plastic surgeons. Cleft palate and lip together is detected with the percentage of 46% among cleft palate and lip patient population. The isolated cleft palate rate is around 33%. Cleft palate and lip most commonly affect men, while isolated palate clefts primarily affect women [1,2,8].
Optimal timing for cleft palate repair is that it should be done to provide normal velopharyngeal function and optimum speech levels, while preserving the development of the face. Therefore, there is a consensus on the practice of palatal repair before 18 months of age to provide a clear speech [4,9].
Different surgical techniques can be applied to cleft palate repair. These techniques, known as primary palatoplasty techniques, include Veau-Wardill-Kilner palatoplasty (Push back), Bardach 2-flap palatoplasty, von Langenbeck palatoplasty (simple palatoplasty), and Furlowpalatoplasty [3,10,11]. In our study, V-Y pushback (77.7%), Simple Palatoplasty (13.8%) and Furlow palatoplasty (8.3%) were applied. The number of the techniques applied was evenly distributed between the groups.
Complications such as bleeding, respiratory distress, infections, dehiscence, and oronasal fistula formation may occur after cleft palate repair. Although bleeding is a rare complication, re-intubation may be required for hemostasis. In addition, excessive bleeding can lead to life-threatening respiratory distress [11-13].
Oronasal fistulas are difficult to treat with a possibility of recurrence. The incidence of fistula formation varies between 5 and 34%. According to the size of the fistula, it is clinically important, when it causes nasal air escape, speech impairment, hearing loss, and regurgitation of food&beverage, and requires re-operation [3,4,13].
Phua and Chala in reported that the rate of fistula in relation to cleft grade was 12.8% in 211 patients and that fistula development was not associated with sex and surgical technique applied [12].
In another study conducted by Sullivan and Marinnan including 449 patients, the patients were operated using two-flap palatoplasty techniques and the fistula rate was found to be 2.9%. The authors reported that fistula formation was related to cleft type rather than operation time, and that fistulas were mostly seen in Veau type 2 and 4 [13].
In another study of 176 cleft palate patients, the fistula rate was found to be 7%, and it was reported that this ratio varied depending on the cleft size and the surgeon’s experience [14]. The authors concluded that the development of fistula was not related to age and sex of the patient, and frequently occurred in the junction of the hard-soft palate [15].
The main causes of oronasal fistula development include poor surgical technique, tense closure, infections, and foreign body irritation [16-18].
Considering the factors leading to the formation of a fistula, it is thought tha the application of closed dressing applied to the wound are as of the other operation fields and the wounds is useful. Thus it is planned to decrease the risk of infection and foreign body irritation by disconnecting with the oral cavity and external environment by closed dressing.
In our study, considering the cause of oronasal fistulas, only primary palatoplasty was applied to 70 patients in Group 1 and the rate of fistula was found to be 7.14%. In Group 2, the cleft was closed with a medium-sized sponge following primary palatoplasty and the rate of fistula was found to be 2.7%. The age distribution of the patients, defect size, and techniques applied were similar in both groups. There was a significant difference between the two groups in terms of oronasal fistula ratios.
Adjusting the size of the gauze is crucial in order to avoid not only airway obstruction and respiratory distress but also preventsagging of the gauze. No other limiting factor was identified in practice.
In conclusion, the use of gauze closure after the operation of palate as a new technique ensures that the flap sticks firmly to the palatal bone and functions as a barrier to prevent contact with food and foreign objects, reducing the risk of infectionand the rate of oronasal fistulas.
In our study, gauze application and fistula ratios were compared between similar groups and further studies have been planning regarding the effect of gauze application on fistula rates according to surgical technique or cleft type.
All of the authors declare that they have all participated in the design, execution, and analysis of the paper, and that they have approved the final version. Additionally, there are no conflicts of interest in connection with this paper, and the material described is not under publication or consideration for publication else where.
Presented in the 32th Congress of Turkish Society of Plastic, Reconstructive and Aesthetic Surgery, September 15-19, 2010, Trabzon, Turkey.
- Kirschner RE, Wang P, Jawad AF (2009) Cleft-palate repair by modified Furlow double opposing Z-plasty: The Children’s Hospital of Philadelphia experience. Plast Reconstr Surg 104: 1998-2002. Link: https://tinyurl.com/y5f2869k
- Muzaffar AR, Byrd HS, Rohrich RJ, Johns DF, LeBlanch D, et al. (2001) Incidence of cleft palate fistula: An institutional experience with two stage palatal repair. Plast Reconstr Surg 108: 1515-1518. Link: https://tinyurl.com/y68qmx7s
- Onah II, Opara KO, Olaitan PB, Ogbonnaya IG (2008) Cleft lip and palate repair: the experience from two West African sub-regional centers. Journal of Plastic, Reconstructive & Aesthetic Surgery 61: 879-882. Link: https://tinyurl.com/y3tqqbdl
- Bekerecioğlu M, Işık D, Bulut Ö (2005) Comparison of the rate of palatal fistulation after two-flap and four-flap palatoplasty. Scand J Plast Reconstr Surg Hand Surg 39: 287-289. Link: https://tinyurl.com/y3bgmbs6
- Emory RE, Clay RP, Bite U, Jackson IT (1997) Fistula formation and repair after palatal closure: An institutional perspective. Plast. Reconstr Surg 99: 1535-1538. Link: https://tinyurl.com/y3j93xvw
- Leow AM, Lun-JouLo LJ (2008) Palatoplasty: Evolution and Controversies. Chang Gung Med J 31: 335-345. Link: https://tinyurl.com/yyf2h74j
- Batchelor AG, Palmer JH (1990) A novel method of closing a palatal fistula: The free fascial flap. Br J Plast Surg 43: 359-362. Link: https://tinyurl.com/yxo8fr2l
- Smith D, Vecchione L, Jiang S, Ford M, Deleyiannis FW, et al. (2007) The Pittsburgh Fistula Classification System: A standardized scheme for the description of palatal fistulas. Cleft Palate Craniofac J 44: 590-594. Link: https://tinyurl.com/y6gmrmjh
- Kirschner RE, Cabiling DS, Slemp AE, Siddiqi F, LaRossa DD, et al. (2006) Repair of oronasal fistulae with acellular dermal matrices. Plast Reconstr Surg 118: 1431-1440. Link: https://tinyurl.com/y6x7v9eu
- Bindingnavele VK, Bresnick ST, Urata MM, Huang G, Leland HA, et al. (2008) Superior Results Using the Islandized Hemipalatal Flap in Palatoplasty: Experience with 500 Cases. Plast Reconstr Surg 122: 232-239. Link: https://tinyurl.com/y58pmk98
- Chapman KL, Hardin-Jones MA, Goldstein JA, Halter KA, Havlik RJ, et al. (2008) Timing of palatal surgery and speech outcome. Cleft Palate Craniofac J 45: 297-308. Link: https://tinyurl.com/y64su3l5
- Phua YS, Chalain T (2008) Incidence of oronasal fistulae and velopharyngeal insufficiency after cleft palate repair: an audit of 211 children born between 1990 and 2004. Cleft Palate Craniofac J 45: 172–178. Link: https://tinyurl.com/y2bx2qyn
- Sullivan SR, Marrinan MD, LaBrie RA, Rogers GF, Mulliken JB (2009) Palatoplasty Outcomes in Nonsyndromic Patients With Cleft Palate: A 29-Year Assessment of One Surgeon’s Experience The Journal of Craniofacial Surgery 20: 612-616. Link: https://tinyurl.com/y5gj26hw
- Lu Y, Shi B, Zheng Q, Hu Q, Wang Z (2010) Incidence of palatal fistula after palatoplasty with levator veli palatine retropositioning according to Sommerlad. British Journal of Oral and Maxillofacial Surgery 10: 637-640. Link: https://tinyurl.com/y2o3eu7h
- Nishio J, Yamanishi T, Kohara H, Hirano Y, Sako M, et al. (2010) Early two-stage palatoplasty using modified Furlow’s veloplasty. Cleft Palate Craniofac J 47: 73-81. Link: https://tinyurl.com/y3nnvb8u
- Çelebiler Ö, Ersoy B, Numanoğlu A (2011) Anterior pillar plasty: a modification in cleft palate repair. J Craniofac Surg 22: 1432-1434. Link: https://tinyurl.com/y6zxmode
- Losken HW, Van Aalst JA, Teotia SS, Dean SB (2011) Achieving low cleft palate fistula rates: surgical results and techniques. Cleft Palate Craniofac J 48: 312-320. Link: https://tinyurl.com/y6zwh52h
- Katzel EB, Basile P, Koltz PZ, Marcus JR, Girotto JA (2009) Current surgical practices in cleft care: cleft palate repair techniques and postoperative care. Plast Reconstr Surg 124: 899-906. Link: https://tinyurl.com/y6d23plr
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
