International Journal of Oral and Craniofacial Science
Palatal pedicle graft for management of a severe case of black triangle: A case report
Saket Kashyap1*, Siddharth Rai2, Sandeep JN3 and Sushama R Galgali4
2Post Graduate Student, Department of Conservative Dentistry and Endodontics, Vokkaligara Sangha Dental College and Hospital, India
3Reader, Department of Periodontics, Vokkaligara Sangha Dental College and Hospital, India
4Professor and Head, Department of Periodontics, Vokkaligara Sangha Dental College and Hospital, India
Cite this as
Kashyap S, Rai S, Sandeep JN, Galgali SR (2019) Palatal pedicle graft for management of a severe case of black triangle: A case report. Int J Oral Craniofac Sci 5(1): 020-023 DOI: 10.17352/2455-4634.000040Development of black triangles following surgical periodontal therapy in severe cases of periodontitis is a common complication faced by patients and clinicians. Restoring the natural form of the interdental area is of utmost importance especially when the anterior aesthetic zone is involved. A wide variety of approaches have been advocated to manage such aesthetic endeavours, which range from soft tissue manipulation to masking with restorative materials. However, the management of black triangles, particularly in cases of treated severe periodontal disease, requires a multidisciplinary approach to recreate the papillary anatomy. This presentation is a case report on management of a case with severe papillary recession occurring after flap surgery. The patient was treated with a combined approach with papilla reconstruction surgery using Coronally Advanced Flap (CAF) and Palatal Pedicle Rotation (PPR) graft and direct composite build-up.
Introduction
The interdental papilla is the part of gingival tissue that occupies the interdental space between two teeth. A number of factors contribute to the shape and size of the interdental gingiva. These factors include the shape and size of the tooth, the position of the tooth in the arch, the anatomy of the contact point and the volume of the gingival tissue. The interdental papilla is an important component of dental aesthetics [1-3]. Loss of the interdental papilla can occur due to a number of etiological factors such as trauma, plaque associated lesions or due to variation in the hard tissue morphology [4].
A number of surgical and non-surgical techniques have been advocated for the management of black triangles. Non-surgical techniques includes the correction of traumatic oral hygiene procedures [4], restoration of the abnormal tooth morphology [5], orthodontic therapy [6] and repeated curettage [7]. Other approaches include the use of hyaluronic acid and the use of gingival mask to cover the interdental spaces for optimum aesthetic results [8,9]. Surgical approach for the management of black triangles includes preservation of papilla during periodontal surgery and reconstruction of lost papilla [4].
Reconstruction of lost papilla has been performed using various techniques involving the surgical manipulation of the interdental tissue to the use of grafts in the interdental area. However, the results obtained by these procedures are unpredictable. The 5-mm rule given by Tarnow et al. in his iconic study, states that when the distance from the contact point to the interproximal osseous crest is 5 mm or less, there is complete fill of the gingival embrasures with an interdental papilla. For every 1 mm above 5 mm, the chance of complete fill is progressively reduced by 50%. Thus management of lost interdental papilla becomes more challenging when there is extensive loss of interdental bone [3].
This case report presents an interdisciplinary approach for the management of a severe case of black triangle. The management of the lost inter dental papilla was done by a rotational pedicle connective tissue graft (RPCTG) followed by direct composite build-up of the tooth involved, in order to attain desired result.
Case Presentation
Clinical presentation
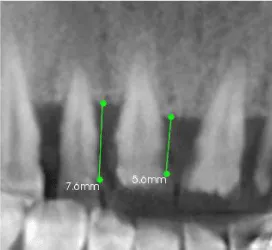
A 29 years old female patient reported to the department of periodontics, Vokkaligara Sangha Dental College and Hospital with the chief complaint of spacing between the upper front teeth. A comprehensive periodontal examination revealed presence of deep periodontal pockets in the maxillary anterior region with presence of subgingival calculus. Also there was loss of interdental papilla between teeth #11 and #12 (Class IV) and #12 and #13 (Class IV).Cone bean computed tomography (CBCT) was done to evaluate the amount of bone support in the maxillary anterior region. CBCT was also used to measure the distance from the bone crest to the cemento enamel junction (CEJ) (Figures 1,2) [10]. The mean distance from the CEJ to the alveolar bone crest, measured on CBCT was 6.6mm. There was also horizontal bone loss & the anterior teeth were grade I mobile
Case management
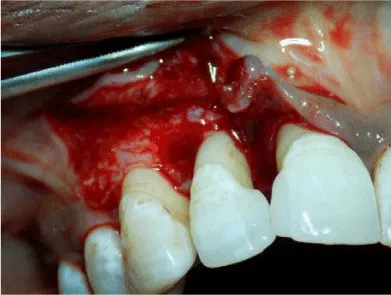
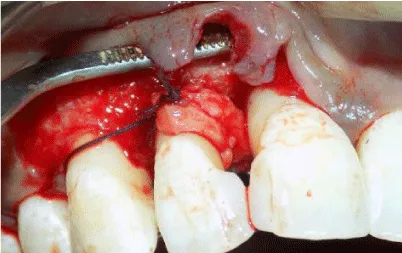
Patient was explained about the treatment plan and written consent was taken from the patient. Phase 1 therapy was completed & patient was re-evaluated a month later for evaluation of the periodontal status. Owing to persistence of pockets in the maxillary anterior region, periodontal flap surgery was carried out .On flap reflection, extensive loss of bone was visible along with reversal of bone architecture (Figure 3). Area was debrided, roots planed & flaps were repositioned & sutured using 5-0 black braided silk sutures. Patient was kept on periodic follow up.
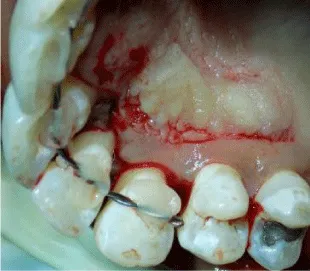
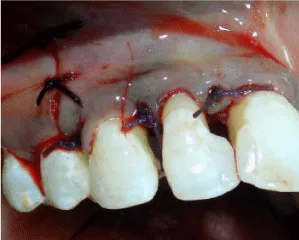
4 months after flap surgery, there was an overall improvement in the quality of gingival tissue but there was no increase in papillary height & persistence of tooth mobility. Splinting of the upper anterior teeth was done & patient was evaluated for papilla reconstruction procedure (Figure 4). Hence papilla reconstruction surgery was planned. On the day of surgery, after administration of local anaesthesia, sulcular incision was given around tooth #11,#12,#13. Papilla between #11 and #12 was preserved by partial thickness modified papilla preservation approach. A vertical incision from the distal line angle of canine extending up to the mucogingival junction was given to help flap mobilization (Figures 5,6).
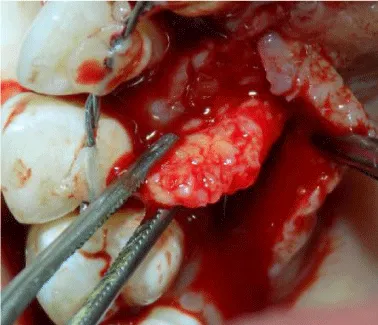
For harvesting the RPCTG, an incision was made on the palate extending from the distal aspect of #15 to the mesial aspect of #11. Epithelial tissue was reflected using a sharp dissection and a pedicle graft was obtained. The graft was free from the distal aspect and intact from the mesial aspect for ease of rotation (Figures 7,8). The RPCTG was then rotated between the interdental space of teeth #11 and #12 and stabilized with a sling suture (Figure 9). The buccal flap was then coronally advanced and stabilized using sling sutures. The vertical incision was closed by interrupted sutures (Figure 10).
Patient was evaluated after 3 months. The gain in the papillary height was not significant (Figure 11). Direct composite build-up in the interdental space was performed using light cure composite. Patient was recalled after one week for finishing and polishing of the restoration. Patient was later recalled after 3 months for evaluation. Clinical photographs at baseline and at 6 months were compared.
Clinical outcome
Although there was 0.5mm increase in papillary height 3 months following surgery, significant changes were observed after the aesthetic composite build up.However, the papillary tissue developed a more biological shape 6 months post operatively. There was also increase in the papillary height at 6 months (Figure 11). The papillary height gain increased from 0.5 mm at 3 months to 2.5 mm at 6 months post operatively. There was an overall improvement in the quality and quantity of interdental tissue between #11 and #12 with a significant overall improvement in the aesthetic outcome (Figures 1,12)
Discussion
With a shift towards achieving aesthetically acceptable results, periodontal therapy has been slowly and gradually moving towards an interdisciplinary approach. A more holistic approach towards the management of defects of the periodontium helps the clinician to not only eliminate active disease, but also retain the natural architecture of the periodontal tissue. The use of composite resin for management of black triangles has been documented in the literature.
Selection of a single approach to manage a complicated defect is not the best treatment approach towards a case, especially in a case where there has been extensive loss of periodontal support due to periodontal disease. Such cases need to be addressed with multiple approaches with each approach contributing for predictable improvement of the outcome. Hence we used a combined approach which involved the use of surgery & synthetic materials. Relocation of the contact point helped in enhancing the surgical outcome resulting in significant improvement in the tissue architecture leading to a biologically sound and aesthetically pleasant presentation [11,12]. Patient motivation is also an important aspect of success of therapy. Such a factor becomes even more relevant when immediate outcomes are not satisfactory. Thus, keeping the patient motivated for regular follow ups and treatment is an important aspect for successful outcome [13].
Patients with severe case of periodontitis often are asymptomatic. In severe case of periodontitis, periodontal surgery arrests the progression of disease & restores the health of the periodontium bur with poor aesthetic outcomes due to post-surgical recession. This may demotivate the patient to seek further treatment. Pocket therapy combined with aesthetic surgical procedures results in a favourable outcome which keeps the patient motivated for maintenance of oral health [14].
Conclusion
The RPCTG associated with a coronally advanced flap along with aesthetic direct composite restoration propitiated a satisfactory improvement in the aesthetic appearance of the patient. Thus, this procedure seems to be a viable approach for the treatment of missing papilla. Further investigation focusing on the clinical effects and predictability of this procedure is required.
- De Castro Pinto RC, Colombini BL, Ishikiriama SK, Chambrone L, Pustiglioni FE, et al. (2010) The subepithelial connective tissue pedicle graft combined with the coronally advanced flap for restoring missing papilla: A report of two cases. Quintessence Int 41: 213-220. Link: https://tinyurl.com/y4tzqs6q
- Zetu L, Wang HL (2005) Management of inter-dental/interimplant papilla. J Clin Periodontol 32: 831-839. Link: https://tinyurl.com/y5p9z6td
- Tarnow DP, Magner AW, Fletcher P (1992) The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol 63: 995-996. Link: https://tinyurl.com/y6rp73kh
- Singh VP, Uppoor AS, Nayak DG, Shah D (2013) Black triangle dilemma and its management in esthetic dentistry. Dental research journal 10: 296-301. Link: https://tinyurl.com/y5bjo5bu
- Blatz MB, Hürzeler MB, Strub JR (1999) Reconstruction of the lost interproximal papilla--presentation of surgical and nonsurgical approaches. Int J Periodontics Restorative Den 19: 395-406. Link: https://tinyurl.com/yyfzl8mk
- Han TJ, Takei HH (1996) Progress in gingival papilla reconstruction. Periodontology 2000 11: 65-68. Link: https://tinyurl.com/yyksnhsk
- Shapiro A (1985) Regeneration of interdental papillae using periodic curettage. The International journal of periodontics & restorative dentistry 5: 26-33. Link: https://tinyurl.com/y64awqah
- Tanwar J, Hungund SA (2016) Hyaluronic acid: Hope of light to black triangles. Journal of International Society of Preventive & Community Dentistry 6: 497-500. Link: https://tinyurl.com/y4r5bfcv
- Ravishankar Y, Srinivas K, Sharma SK, Shameen KP (2012) Management of Black Triangles and Gingival Recession: A Prosthetic Approach. Indian Journal of Dental Sciences 4: 141-145. Link: https://tinyurl.com/y2bjeh46
- Nordland WP, Tarnow DP (1998) A classification system for loss of papillary height. J Periodontol 69: 1124-1126. Link: https://tinyurl.com/yy33t5t3
- Wu YJ, Tu YK, Huang SM, Chan CP (2003) The influence of the distance from the contact point to the crest of bone on the presence of the interproximal dental papilla. Chang Gung med j 26: 822-828. Link: https://tinyurl.com/yyholf6l
- Wahbi MA, Al Sharief HS, Tayeb H, Bokhari A (2013) Minimally invasive use of coloured composite resin in aesthetic restoration of periodontially involved teeth: Case report. The Saudi dental journal 25: 83-89. Link: https://tinyurl.com/y5nw5ljw
- Pac A, Oruba Z, Olszewska-Czyż I, Chomyszyn-Gajewska M (2014) The significance of motivation in periodontal treatment: validity and reliability of the motivation assessment scale among patients undergoing periodontal treatment. Community Dent Health 31: 53-56. Link: https://tinyurl.com/y5qcompn
- Hirsch A, Brayer L, Shapira L, Goldstein M (2004) Prevention of gingival recession following flap debridement surgery by subepithelial connective tissue graft: Consecutive case series. J Periodontol 75: 757-761. Link: https://tinyurl.com/yyknbldg
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.







 Save to Mendeley
Save to Mendeley
