International Journal of Oral and Craniofacial Science
Correlation between temporomandibular disorders and malocclusions: A retrospective observational study-can malocclusions or previous orthodontic treatments affect Temporo-Mandibular Disorders?
Alessandro Marchesi*, Dorothea Bellini, Andrea Sardella, Giulia Fornarelli and Tomson Zefi
Cite this as
Marchesi A, Bellini D, Sardella A, Fornarelli G, Zefi T (2022) Correlation between temporomandibular disorders and malocclusions: A retrospective observational study-can malocclusions or previous orthodontic treatments affect Temporo-Mandibular Disorders? Int J Oral Craniofac Sci 8(1): 001-009. DOI: 10.17352/2455-4634.000051Copyright License
© 2022 Marchesi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Background: The purpose of this article is to verify the possible correlation between TMD (Temporomandibular Disorders) and different types of malocclusions in adult subjects and subsequently that between TMD and previous orthodontic treatment.
Materials and methods: A retrospective observational study was conducted in San Paolo e Carlo Hospital, associates of the University of Milan, for a period of 2 years (1st February 2019 – 3rd March 2020), on 374 adult patients (244 females and 130 males). The subjects underwent an intraoral examination with a gnathological assessment, in order to distinguish those who suffered from TMD and those who did not. Secondly, the patients were subjected to orthodontic examination to identify those who had previously undergone orthodontic treatment, assessing through an extraoral and intraoral examination, the dental class, the type of dental bite and the presence or absence of a midline deviation.
Results: The data analysis revealed a statistically significant association between TMD and gender (p= 0.023, OR= 1.66). The association between class I, II, III malocclusions and the presence of TMD was found to be statistically significant: p<0.0001 (OR= 4.04) and that between open/deep bite and the presence of TMD too: p= 0.003 (OR= 1.89). Moreover, the correlation between midline deviation and the presence of TMD was statistically significant: p<0.0001 (OR=7.48). On the other hand, no correlation was found between TMD and previous orthodontic treatment (p= 0.918).
Conclusions: The available data revealed a statistically significant association between TMD and malocclusions, related to dental class and bite and midline deviation, although the existing results in the literature are controversial regarding this association.
While no statistically significant correlation was found between TMD and previous orthodontic treatment. Orthodontic therapy, therefore, by correcting occlusion anomalies, could reduce the risk of TMD incidence. Finally, longitudinal studies with adequate statistical power are needed to clarify the possible interrelationships between TMD and malocclusions.
Abbreviations
TMJ: Temporomandibular Joint; TMD: Temporomandibular Disorders; EMG: Electromyography
Introduction
The study of occlusion and its relationship with the function of the chewing system has been for many years a topic of interest in dentistry. The enormous curiosity in this field in association with the lack of complete knowledge led to the formulation of numerous concepts, theories, and methods of treatment.
The first supposition of a possible relationship between occlusion and TMJ function was suggested by Costen [1], who hypothesized that changes in dental conditions (e.g. loss of vertical dimension or deep bite) can lead to temporomandibular disorders and eventual otological symptoms.
Michelotti [2] proposed that occlusal interference may increase the habitual activity of the jaw muscles and consequently lead to TMD. By means of electromyography (EMG), the effects of an acute occlusion disturbance on habitual muscular activity were investigated. The masticatory system response revealed a reduction in the activity of the masseter muscle, and none of the test subjects showed signs and/or symptoms of TMD. Considering that healthy subjects without parafunctional activity were included in this study, it was hypothesized that the reaction to occlusal disturbances differs in patients with TMD.
Le Bell [3] used the same method implemented in Michelotti’s study to observe the reactions in a group of patients with myofascial pain. The results showed an increase in the habitual activity of the masseter muscle and an increase in masticatory muscle pain. This led to the belief that subjects who were occlusal altered and affected by interference, upped the activity of the masticatory muscles, which in turn led to pain and dysfunction.
Hirsch and John [4,5] investigated the association between overjet and overbite and TMD in a sample of more than 3000 subjects and found no correlation.
Among the various malocclusions, it has been suggested that posterior crossbite may be an important risk factor for TMD [6].
According to Pullinger [7], the possibility of a person with a posterior crossbite having a disc dislocation with reduction ranges from 3.3 to 1 in comparison to the population without crossbite. This does not seem to be true for young patients, in fact, there appears to be no correlation between crossbite and disc dislocation because initially there is a good adaptation [8,9].
Manfredini [10] and his colleagues studied a sample of approximately 400 subjects affected by TMD and did not find an association between malocclusions and TMD.
Evidence of a link between malocclusions and TMD should meet certain criteria. First of all, the causes must precede the effects, whereas, in the literature, we find studies demonstrating the opposite, i.e. that muscular pain causes changes in occlusion [11]. Furthermore, if there is an association, the more severe the malocclusion the more severe the pathology should be. In contrast, the previous studies suggest that the risk of TMD may only be associated with certain malocclusions. The results of the scientific community must be consistent over time, as an increasing number of studies reduce the importance of the role of occlusal factors in the etiology of TMD.
In the light of these considerations, it may be thought that occlusion is not currently to be considered the main risk factor for TMD.
Although there are many conflicting opinions, it was decided to carry out a retrospective observational study to continue investigating in this field [12,13].
In the last decade, in fact, temporomandibular disorders have increased in number and severity, presenting themselves in an even more complex way by being always linked to multifactorial etiopathogenesis. This constituted a reason for a daily confrontation with the patient and an even more accurate anamnesis and first visit.
The primary objective of this study is to investigate the existence of a possible correlation between TMD and different types of malocclusions in adult subjects, focusing on class I malocclusion, which differ from the normal occlusion only in the position of the teeth in relation to the occlusal line but not in the molar relationship [14-16], II and III malocclusions (sagittal plane); open or deep anterior bite (vertical plane); midline deviation.
The secondary objective is to investigate the correlations between the various types of orthodontic treatment and TMD. Orthodontic treatment is usually long-lasting and patients may complain of TMD symptoms before, during, or after treatment. Therefore, interest in the relationship between orthodontic treatment and TMD has grown, and many studies have been conducted on this topic without any solid evidence.
The need to investigate this relationship emerged from the occurrence of legal cases in which patients undergoing orthodontic treatment reported the onset of symptoms and signs of TMD during or after the course of treatment.
A 1995 review by McNamara, Sclingun, and Okeson [17] came up with eight conclusions that refuted this possible association.
The hypothesis that various orthodontic techniques may be involved as etiological factors in TMD has also been tested in recent decades by Dibbets and van der Weele [18], who have concluded that there is no causal relationship between the two.
According to current knowledge, the role of orthodontic treatment in the onset of TMD is not confirmed and the conclusions indicated by McNamara et Al. are still valid.
A meta-analysis in regards identified no studies that indicated a link between traditional orthodontic treatment and an increase in the prevalence of TMD [19].
Other studies have also shown that there is no variation in the incidence of TMD symptoms or signs depending on whether functional or fixed orthodontic therapy is used [20-23].
A review [24] of the international literature has shown that orthodontic treatment, regardless of the technique used and regardless of premolar extraction during treatment, does not increase the signs and symptoms of TMD and is therefore not a risk factor for its development. Orthodontic treatment does not appear to be a valuable resource for treating or preventing the onset of TMD signs and symptoms. There is a need to improve the methodology used in the attempt to demonstrate a possible association between TMD and orthodontic treatment, to resolve the current contradictions.
Materials and methods
This is an observational study, conducted in the Complex Operative Unit of Stomatology and Oral Prevention of the San Paolo e Carlo Hospital, associates of the University of Milan, for a period of 2 years (1st February 2019 – 3rd March 2020) on 374 adult patients (244 females and 130 males). The sequential recruitment of patients attending the examination was carried out according to eligibility criteria. Inclusion criteria were age between 18 and 65 years; non-syndromic patients (patients without chromosomal, monogenic, epigenetic diseases); absence of any cause of intraoral pain (dental, periodontal, etc.).
Exclusion criteria were patients with partial (Class 1 and 2, according to the classification of the American College of Prosthodontists [25]) or total edentulism; patients with removable total dentures, partial dentures, and/or dental implants; patients with tumors in the head and neck region; patients with mandibular fractures; patients who have undergone previous orthognathic surgery.
Table 1 shows the socio-demographic and clinical characteristics of the subjects at recruitment.
The selected subjects underwent a detailed gnathological examination in order to distinguish those with TMD from those without.
Among the 374 subjects examined, 188 subjects did not present TMD at the time of the first visit whereas 186 subjects suffered from TMD.
In addition, all patients were assessed from an orthodontic point of view to distinguish those who had previously undergone orthodontic treatment from those who had not undergone any kind of orthodontic treatment.
A questionnaire was designed to assess the presence or absence of mobile or fixed orthodontic treatment and the age at which this treatment had been carried out, with age ranges of 6-12, 12-19, and >19 years. The questionnaire showed that among the 374 subjects in the sample, 191 had not previously undergone any type of orthodontic treatment, representing the control group, and 183 had, of whom 58 had undergone fixed treatment; 63 had undergone removable treatment; 62 had combined fixed and removable orthodontic treatment.
Finally, they underwent a thorough extraoral, intraoral, and functional clinical examination to assess their dental class, the type of dental bite, and the presence or absence of midline deviation.
During the gnathological examination, the TMJ disorders were analyzed according to the Helkimo clinical dysfunction index [26], which provides specific classifications and scores in order to homogenize and rationalize the various findings and make them comparable with the existing literature.
This index assesses the functional status of the masticatory system, considering: the decreased extension of the measured mandibular movements (opening, protrusion, right and left laterality), noises or joint blocks, deviations in the mandibular pathway, spontaneous pain in one or more movements, palpatory muscle pain (one or more painful points) and palpatory joint pain (lateral pole and posterior pole of the condyle).
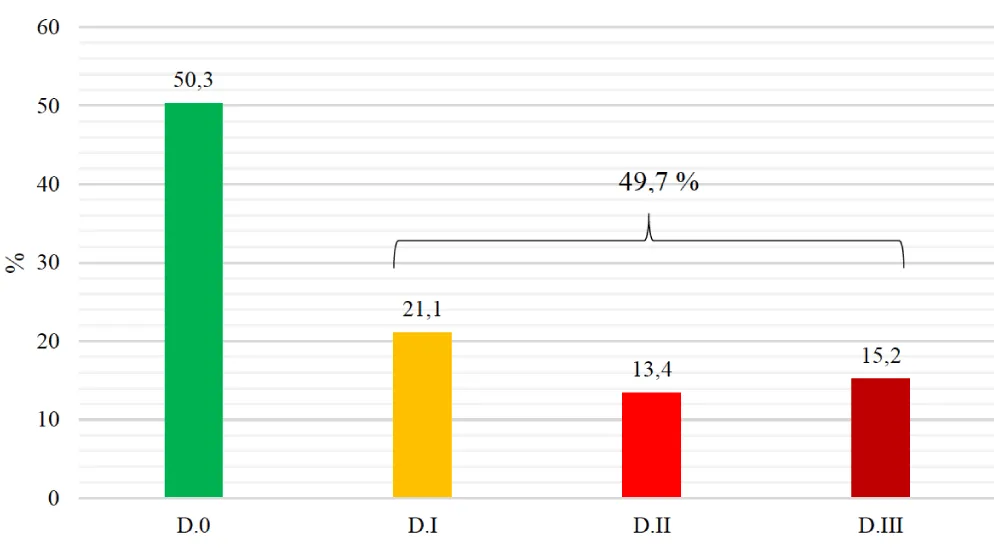
For each of these clinical signs, a score of 0, 1, or 5 points was assigned according to their presence and severity. The classification of clinical dysfunction, based on the collected scores, includes the absence of dysfunction (D.0): 0 points, mild dysfunction (D.I): 1-4 points, moderate dysfunction (D.II): 5-9 points, severe dysfunction (D.III): 10-25 points.
The orthodontic examination was carried out first by an extra-oral clinical examination, which consisted in observing the face from a frontal view identifying the reference midlines (horizontal and vertical).
Subsequently, an intra-oral examination was conducted, assessing intraoral health (general dental condition; periodontal condition; presence of signs of parafunction ). The intraoral examination was completed by the observation of common orthodontic parameters: molar and canine class, overjet, overbite, crossbite, midlines, mandibular deviations in opening and closing.
For overbite, deep bite, and open bite, the US values were taken into account: an overbite value of up to 3mm was considered normal and regarding the open bite and deep bite values, measurements lower than 0mm and greater than 3mm, respectively, were taken into consideration [27].
Incisive and canine guides were also analyzed to assess whether they were well represented or absent.
Regarding the midline, in maximum intercuspation, the upper midline was assessed to the lower midline and vice versa and the position of the single midlines of the two jaws to the facial midline. Assessing the midline coincidence during the opening permits a differential diagnosis between a functional asymmetry and a true asymmetry (skeletal or dental) [28,29].
Finally, during the functional examination, the presence of vicious habits (present or past), the type of breathing, and swallowing was assessed.
Regarding the statistical analysis, descriptive data are expressed as mean, standard deviation (SD), median, range of variability (min-max) for continuous variables, several subjects, and percentage for discrete variables. The comparison between subjects with and without TMD was conducted based on the age by means of Student’s t-test for independent samples, chi-square test or Fisher’s exact test for discrete variables, or the non-parametric Mann-Whitney test. The Odds Ratio (OR) and its 95% confidence interval (95% CI) were also estimated. The association between the degree of TMD severity and the presence of malocclusion and/or previous orthodontic treatment was assessed using the chi-square test or the Kruskal-Wallis test, when appropriate. Finally, a multivariate logistic analysis, adjusted according to sex and age, was conducted to assess whether and which occlusal and orthodontic variables studied were independently associated with TMD. Values below 0.05 of the p-significance level were considered statistically significant (two-tailed test). The SPSS program version 24.0 for Windows (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
Among the 374 subjects examined, 50.3% (188 subjects) did not present TMD at the time of the first visit whereas 49.7% (186 subjects) suffered from TMD.
The prevalence of TMD in the sample was therefore 49.7%, with a confidence interval of 44.7-54.8%.
Figure 1 compares subjects free of TMD (D.0) with subjects affected by TMD. The latter is distributed by the degree of severity, based on Helkimo’s clinical dysfunction index.
Out of the 186 subjects presenting a TMD: 79(21.1%) had mild dysfunction (D. I); 50(13.4%) had a moderate dysfunction (D.II); 57(15.2%) had severe dysfunction (D.III).
Among the 374 subjects in the sample: 191(51.1%) had not previously performed any type of orthodontic treatment; 58(15.5%) had undergone fixed treatment; 63(16.8%) had undergone removable treatment; 62(16.6%) had combined fixed and removable orthodontic treatment.
The prevalence of previous orthodontic treatment in our sample was 48.9% with a confidence interval of 43.9-54%.
The statistical analysis revealed a significant association between TMD and gender.
Of the 244 female subjects: 112(45.9%) had no TMD and 132(54.1%) had TMD. The prevalence of TMD in females was therefore 54.1% with a confidence interval of 47.8-60.2%.
Of the 130 male subjects: 76(58.5%) had no TMD; 54(41.5%) had TMD. The prevalence of TMD in males was 41.5% with a confidence interval of 33.4-50.1%.
Stratified analysis by gender showed a statistically significant difference in the prevalence of TMD between females and males (p= 0.023). The risk of having TMD in females compared to males is thus 1.66 times higher.
On the other hand, the age-stratified analysis showed no statistically significant difference in the prevalence of TMD.
By examining the numerical and percentage distribution of subjects in the sample with or without TMD in relation to orthodontic treatment, no statistically significant association was found (p= 0.918). The evaluation was based on a binomial distribution and a 95% confidence interval (Table 2).
Table 3 shows the distribution of subjects in the sample with and without TMD compared to the presence or absence of malocclusions in the sagittal plane.
69.3% of the subjects in the sample presented a Class I, II, or III malocclusions (according to Angle’s classification). The association between these malocclusions and the presence of TMD was found to be statistically significant: p<0.0001 (OR= 4.04).
The presence of class I, II, and III malocclusions is approximately 50% higher in subjects with TMD than in those without TMD.
Table 4 shows the distribution of subjects in the sample with and without TMD in relation to the dental bite; 42.8% of the subjects had an altered bite (open or deep bite). The association between open/deep bite and the presence of TMD was found to be statistically significant: p=0.003 (OR= 1.89).
The presence of an open or deep bite was approximately 45% greater in subjects with TMD than in those without TMD.
The distribution of subjects in the sample with and without TMD was also analyzed in relation to the deviation of the inter-incisive line (Table 5): 18.7% of the subjects had an inter-incisive line deviation greater than or equal to 3mm. The association between inter-incisive line deviation and the presence of TMD was found to be statistically significant: p<0.0001 (OR= 7.48). The presence of a deviation greater than or equal to 3mm was approximately five times greater in subjects with TMD in comparison to those without TMD.
Table 6 shows the distribution of the subjects in the sample with or without TMD, divided into subgroups, in relation to the four dental classes: Normal Class I, Malocclusion Class I, Malocclusion Class II, and Malocclusion Class III; 0.7% of the sample subjects presented a normal occlusion; 35.6% presented a Class I malocclusion; 20.6% presented a Class II malocclusion; 13.1% presented a Class III malocclusion. The stratified analysis by dental class showed a statistically significant difference in the prevalence of TMD compared to the different types of malocclusions. Respectively: Class I malocclusion: p<0.0001; OR= 2.75; CI 95%: 1.56-4.87. Class II malocclusion: p<0.0001; OR= 6.36; 95% CI: 3.21-12.72. Class III malocclusion: p<0.0001; OR= 6.14; 95% CI: 2.78-13.73.
Subjects with a Class II and III malocclusion had an approximately six-fold increased risk of having TMD.
Table 7 shows the distribution of the subjects in the sample with or without TMD, divided into subgroups, in relation to the three types of bite considered in our study: normal bite, open bite, and deep bite; 7.2% of the sample subjects had a normal bite; 21.2% had an anterior open bite; 21.6% had a deep bite. The stratified analysis by dental bite showed a statistically significant difference in the prevalence of TMD compared to the open and deep bite. Respectively open bite: p= 0.005; OR= 2.17; CI 95%: 1.24-3.81; deep bite: p= 0.067; OR= 1.66; 95% CI: 0.96-2.87.
Subjects with an anterior open bite were more likely to have TMD than those with a deep bite.
Finally, a multivariate logistic analysis, adjusted for gender and age, was conducted to assess whether and which occlusal and orthodontic variables studied were independently associated with temporomandibular disorders (Table 8). The multivariate logistic analysis confirmed an independent association of TMD with sagittal plane malocclusions (class I, II, and III malocclusions) and with midline deviation. On the contrary, the association with vertical malocclusions (open and deep bite) was not statistically significant.
Discussion
In similarity with our study, other research conducted [30-33] on the adult population estimated a prevalence of around 55% for women and around 40% for men. The stratified analysis by sex showed a statistically significant difference in the prevalence of TMD between females and males (p = 0.023) in which female subjects presented about twice the risk of TMD compared to male subjects.
This finding is in agreement with previous studies and confirms what others have already concluded [34,35].
Regarding the age of the subjects in the sample, no statistically significant difference was found in the prevalence of TMD (p=0.322), consistent with other international scientific studies, in which, although there was a trend of greater severity of TMD in young adults, no correlation was found between age and presence of TMD [36-38].
Young adults represent the life stage of greatest production and difficulty. With advancing age comes changes in the standard of living and adaptive capacity of individuals with TMD; signs and symptoms become subclinical and perceived at a lower intensity, resulting in less pronounced severity.
The increasingly early onset of the first signs and symptoms of TMD is mainly due to parafunctional habits [39-41].
In this study, in contrast to what various scientific literature has shown, a statistically significant association emerged between TMD and the malocclusions considered.
Most of the scientific literature in fact shows a weak link between malocclusions and TMD [42] or a total absence of causal relationship [43].
The association between class I, II, and III malocclusions (according to the Angle classification) and the presence of TMD was found to be statistically significant (p<0.0001). According to the data obtained, subjects with a Class II and III malocclusion are six times more likely of having TMD than subjects with a normal class I. On the contrary, subjects with a Class I malocclusion are roughly three times more susceptible to having TMD than subjects with a normal Class I.
The association between malocclusions in the vertical plane (open and deep bite) and the presence of TMD was found to be statistically significant (p=0.003). According to the data obtained, subjects with an anterior open bite are more likely to have TMD than those with a deep open bite. These results support those obtained by Michelotti [2] (2005) and by LeBell [3] (2006) who both studied the muscle activity of the chewing system in patients with malocclusions.
The association between midline deviation greater than or equal to 3mm and the presence of TMD was found to be statistically significant (p<0.0001). The presence of a deviation greater than or equal to 3mm was approximately five times greater in subjects with TMD than in those without TMD.
No statistically significant correlation was found between TMD and previous orthodontic treatments, confirming the results reported by international literature and in particular, the results obtained in the study conducted by McNamara, Slingun, Okeson [17] in 1995, whose concepts are still considered clinically valid today.
Furthermore, as an observational study, it is not possible to draw any etiological conclusions on the possible relationship between TMD and malocclusions. Longitudinal studies with adequate statistical power and tools capable of diagnosing and dividing TMD into subtypes (such as muscular, articular, and mixed), appear to be necessary for a better understanding of this association.
Conclusion
In conclusion, the results of this retrospective observational study, conducted on an adult population, suggest the existence of a statistically significant association between TMD and malocclusions, related to dental class, type of dental bite, and midline deviation.
In contrast to the literature [44,45], in this study the open bite seems to be associated with TMD much more than the deep bite: this could be due to the lack of anterior guides in open bites, in which the mandible is freer to move, and this can more easily lead to the onset of TMD than in those who have a deep bite with canine and incisor guides that are more accentuated.
Furthermore, all malocclusions (class I, II, III) are associated with TMD and this could be explained by the lack of anterior guides (as in open bite), which leads to joint overloading and, consequently, to the onset of TMD. This hypothesis is strengthened by the fact that the correlation between malocclusions and TMD was not only associated with second and third-class malocclusions, where the problem would be only the sagittal defect, but also with first-class molars with dysfunction in the guides. Thus, guidance interference could play an important role in the occurrence of TMD.
The association that has been demonstrated between midline deviation >3mm and the onset of TMD could be due to a positional problem of the mandible and therefore to a discrepancy between centric relation and maximum intercuspation , with consequent later mandibular deviation, which could lead to the genesis of TMD [46].
The same correlation cannot be deduced for orthodontic treatment: although it overloads the TMJ during therapy, after some time it does not affect the TMJ and the genesis of TMD.
This could be a strong suggestion that orthodontic therapy should be used for the resolution of all types of malocclusions, in order to reduce the risk of incidence of TMD.
The strength of this study is that it significantly demonstrates that malocclusions are associated with TMD and orthodontic treatment can be a protective factors for the occurrence of TMD.
Nevertheless, it would be ideal to have an even larger sample available in order to better analyze the different severities of TMD and the different types of orthodontics (mobile/fixed) and ages of intervention.
Another limitation might be that no cases with aligner orthodontics were included, which should be investigated in further studies.
Authors’ contributions
Dorothea Bellini, Giulia Fornarelli e Tomson Zefi have given substantial contributions to the acquisition of the data, Alessandro Marchesi and Andrea Sardella have contributed to the analysis and interpretation of the statistical data and to the conception of the manuscript. All authors have participated in drafting the manuscript, Alessandro Marchesi revised it critically. All authors read and approved the final version of the manuscript.
All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
All authors read and approved the final version of the manuscript.
- Costen JB (1997) A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. 1934. Ann Otol Rhinol Laryngol 106: 805-819. Link: https://bit.ly/3Jye1z2
- Michelotti A, Farella M, Gallo LM, Veltri A, Palla S, et al. (2005) Effect of occlusal interference on habitual activity of human masseter. J Dent Res 84: 644-648. Link: https://bit.ly/3rTBlkS
- Le Bell Y, Niemi PM, Jämsä T, Kylmälä M, Alanen P (2006) Subjective reactions to intervention with artificial interferences in subjects with and without a history of temporomandibular disorders. Acta Odontol Scand 64: 59-63. Link: https://bit.ly/3oVDCtV
- John MT, Hirsch C, Drangsholt MT, Mancl LA, Setz JM (2002) Overbite and overjet are not related to self-report of temporomandibular disorder symptoms. J Dent Res 81: 164-169. Link: https://bit.ly/34LVQav
- Hirsch C, John MT, Drangsholt MT, Mancl LA (2005) Relationship between overbite/overjet and clicking or crepitus of the temporomandibular joint. J Orofac Pain 19: 218-225. Link: https://bit.ly/3HUr79D
- Lippold C, Hoppe G, Moiseenko T, Ehmer U, Danesh G (2008) Analysis of condylar differences in functional unilateral posterior crossbite during early treatment--a randomized clinical study. J Orofac Orthop 69: 283-296. Link: https://bit.ly/3uUnaOz
- Pullinger AG, Seligman DA, Gornbein JA (1993) A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res 72: 968-979. Link: https://bit.ly/3BmzPeh
- Farella M, Michelotti A, Iodice G, Milani S, Martina R (2007) Unilateral posterior crossbite is not associated with TMJ clicking in young adolescents. J Dent Res 86: 137-141. Link: https://bit.ly/3LDxyjy
- Khayat N, Winocur E, Kedem R, Winocur Arias O, Zaghal A, et al. (2021) The Prevalence of Temporomandibular Disorders and Dental Attrition Levels in Patients with Posterior Crossbite and/or Deep Bite: A Preliminary Prospective Study. Pain Res Manag Link: https://bit.ly/3oTd906
- Manfredini D, Perinetti G, Guarda-Nardini L (2014) Dental malocclusion is not related to temporomandibular joint clicking: a logistic regression analysis in a patient population. Angle Orthod 84: 310-315. Link: https://bit.ly/34M05CX
- Obrez A, Stohler CS (1996) Jaw muscle pain and its effect on gothic arch tracings. J Prosthet Dent 75: 393-398. Link: https://bit.ly/3va0CcP
- Mohlin B, Axelsson S, Paulin G, Pietilä T, Bondemark L, et al. (2007) TMD in relation to malocclusion and orthodontic treatment. Angle Orthod 77: 542-548. Link: https://bit.ly/34WbGz0
- Egermark I, Magnusson T, Carlsson GE (2003) A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. The Angle orthodontist 73: 109-115. Link: https://bit.ly/3uRKXyz
- Proffit W (2013) Ortodonzia moderna, Elservier Masson Srl 38-39.
- Angle EH (1899) Classification of malocclusion. Dent Cosmos 41: 248-264.
- Brown T, Townsend GC, Richards LC, Burgess VB (1990) Concepts of occlusion: Australian evidence. Am J Phys Anthropol 82: 247-256. Link: https://bit.ly/34E0Tda
- McNamara Jajr, Seligman DA, Okeson JP (1995) Occlusion, Orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain 9: 73-90. Link: https://bit.ly/3oPlbY0
- Dibbets JM, Van der Weele LT (1992) Long-term effects of orthodontic treatment, including extraction, on signs and symptoms attributed to CMD. Eur J Orthod 14: 16-20. Link: https://bit.ly/3gR1vi0
- Kim MR, Graber TM, Viana MA (2002) Orthodontics and temporomandibular disorder: a meta-analysis. Am J Orthod Dentofacial Orthop 121: 438-446. Link: https://bit.ly/3gPZ3bn
- Janson M, Hasund A (1981) Functional problems in orthodontic patients out of retention. Eur J Orthod 3: 173-179 Link: https://bit.ly/3HThDv6
- Keeling SD, Wheeler TT, King GJ, Garvan CW, Cohen DA, et al. (1998) Anteroposterior skeletal and dental changes after early Class II treatment with bionators and headgear. Am J Orthod Dentofacial Orthop 113: 40-50. Link: https://bit.ly/3uQbWKR
- Jos MHD , David SC (1995) Implications of temporomandibulardisorders for facial growth and orthodontic treatment. Seminars in Orthodontics 1: 258-272. Link: https://bit.ly/3HT8Wkz
- Luther F (1998) Orthodontics and the temporomandibular joint: where are we now? Part 1. Orthodontic treatment and temporomandibular disorders. Angle Orthod 68: 295-304. Link: https://bit.ly/3rV4uwd
- Leite RA, Rodrigues JF, Sakima MT, Sakima T (2013) Relationship between temporomandibular disorders and orthodontic treatment: a literature review. Dental Press J Orthod 18: 150-157. Link: https://bit.ly/3BqYIWj
- McGarry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR, et al. (2002) Classification system for partial edentulism. J Prosthodont 11: 181-193. Link: https://bit.ly/3JtzJnW
- Helkimo M (1974) Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven Tandlak Tidskr 67: 101-121. Link: https://bit.ly/3GT5J38
- Celikoglu M, Akpınar S, Yavuz I (2010) The pattern of malocclusion in a sample of orthodontic patients from Turkey. Med Oral Patol Oral Cir Bucal 15: 791-796. Link: https://bit.ly/3Bo72Gf
- Bishara SE, Burkey PS, Kharouf JG (1994) Dental and facial asymmetries: a review. Angle Orthod 64: 89-98. Link: https://bit.ly/3HOox4R
- Lin H, Zhu P, Lin Y, Wan Y, Shu X, et al. (2013) Mandibular asymmetry: a three-dimensional quantification of bilateral condyles. Head & Face Medicine 9: 42. Link: https://bit.ly/34FvLtN
- Espinosa De Santillana IA, Garcia MA, Garcia VAM, Ogaqa TR (2013) Severity index by gender in adult patients with Temporo-mandibular Disorders (TMD). International Journal of Medicine and Medical Sciences 3: 321-327. Link: https://bit.ly/3uZM0g1
- Rollman GB, Lautenbacher S (2001) Sex differences in musculoskeletal pain. Clin J Pain 17: 20-24. Link: https://bit.ly/3oVJGCH
- Tsang A, Von Korff M¸ Lee S, Alonso J, Karam E, et al. (2008) Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 9: 883-891. Link: https://bit.ly/352XHHO
- Suvinen TI, Reade PC, Hanes KR, Könönen M, Kemppainen P (2005) Temporo-mandibular medisorder subtypes according to self-reported physical and psychoso-cial variables in female patients: a re-evaluation. J Oral Rehabil 32: 166-173. Link: https://bit.ly/3LDnS8H
- Mušanović A, Ajanović M, Redžepagić Vražalica L, Kazazić L, et al. (2021) Prevalence of TMD among Children Provided with Fixed Orthodontic Treatment. Acta Stomatol Croat 55: 159-167. Link: https://bit.ly/3gRR2me
- Lai YC, Yap AU, Türp JC (2020) Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J Oral Rehabil 47: 270-280. Link: https://bit.ly/34M199V
- Mazzetto MO, Rodrigues CA, Magri LV, Melchior MO, Paiva G (2014) Severity of TMD related to age, sex and electromyographic analysis. Braz Dent J 25: 54-58. Link: https://bit.ly/34E1gEA
- Mazzetto MO, Rodrigues CA, Magri LV, Melchior MO, Paiva G (2014) Severity of TMD related to age, sex and electromyographic analysis. Braz Dent J 25: 54-58. Link: https://bit.ly/3uVAkL4
- Karibe H, Goddard G, Shimazu K, Kato Y, Warita-Naoi S, et al. (2014) Comparison of self-reported pain intensity, sleeping difficulty, and treatment outcomes of patients with myofascial temporomandibular disorders by age group: a prospective outcome study. BMC Musculoskelet Disord 15: 423. Link: https://bit.ly/3LDnSFJ
- Da Silva GG, Pachêco-Pereira C, Porporatti AL, Savi MG, Peres MA, et al. (1939) Prevalence of clinical signs of intra-articular temporomandibular disorders in children and adolescents: A systematic review and meta-analysis. Journal of the American Dental Association 147: 10-18.e8. Link: https://bit.ly/3GO0eTb
- Dibbets JM (1977) Juvenile temporomandibular joint dysfunction and craniofacial growth: A statistical analysis. Link: https://bit.ly/34WcXWO
- Cortese SG, Fridman DE, Farah CL, Bielsa F, Grinberg J, et al. (2013) Frequency of oral habits, dysfunctions, and personality traits in bruxing and nonbruxing children: a comparative study. Cranio 31: 283-290. Link: https://bit.ly/3HVBM3O
- Michelotti A, Rongo R, D'Antò V, Bucci R (2020) Occlusion, orthodontics, and temporomandibular disorders: Cutting edge of the current evidence. J World Fed Orthod 9: S15-S18. Link: https://bit.ly/3LCEu0a
- Manfredini D, Lombardo L, Siciliani G (2017) Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil 44: 908-923. Link: https://bit.ly/3Jv2oc5
- Liu JK, Tsai MY (1997) Relationship between morphologic malocclusion and temporomandibular disorders in orthodontic patients prior to treatment. Funct Orthod 14: 13-16. Link: https://bit.ly/3uYqrw7
- Marangoni AF, de Godoy CH, Biasotto-Gonzalez DA, Alfaya TA, Fernandes KP, et al. (2014) Assessment of type of bite and vertical dimension of occlusion in children and adolescents with temporomandibular disorder. J Bodyw Mov Ther 18: 435-440. Link: https://bit.ly/3Bns87q
- D'Ippolito S, Ursini R, Giuliante L, Deli R (2014) Correlations between mandibular asymmetries and temporomandibular disorders (TMD). Int Orthod 12: 222-238. Link: https://bit.ly/3s1Z6rf
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
