International Journal of Oral and Craniofacial Science
Commentary-practicing state of the art occlusion in the Digital Era of Dentistry
Kerstein RB*
Cite this as
Kerstein RB (2022) Commentary-practicing state of the art occlusion in the Digital Era of Dentistry. Int J Oral Craniofac Sci 8(1): 015-019. DOI: 10.17352/2455-4634.000053Copyright License
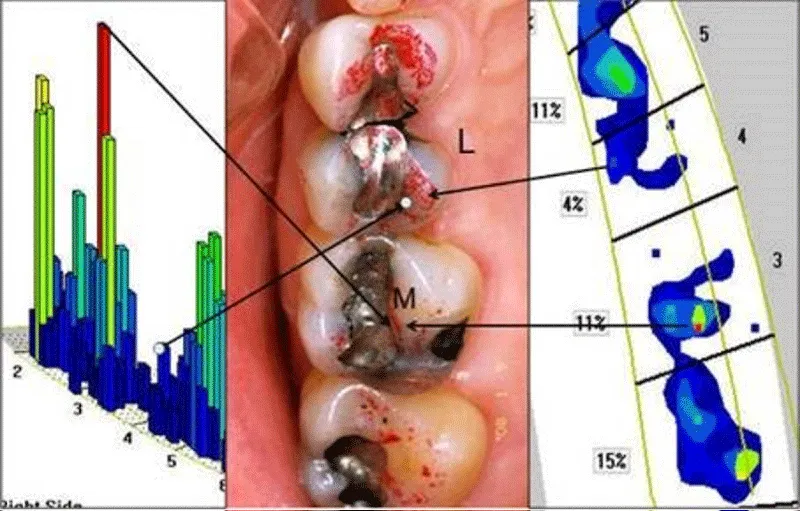
© 2022 Kerstein RB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.New technological developments in modern dental medicine offer clinicians insight and treatment advances to many outdated, dogmatic concepts that have been widely believed for many years, despite there being a lack of scientific evidence to support them. This is especially true in the field of Dental Occlusion, whose scientific development has been hampered by the use of traditional, non-digital occlusal indicators that do not quantify occlusion, other than possibly describing “contact area”. Yet, the literature continues to suggest that dentists can visually observe the size of holes in wax or silicone, the size and color depth of articulating paper marks, or judge shim stock hold between occluding teeth, as being reliable methods to describe occlusal force levels, when research shows these traditional “beliefs” are scientifically untrue [1-3]. And despite having no scientific validity, articulating paper mark size continues to be the “Standard of Care” to analyze occlusal contact forces. Presently, no published study shows articulating paper marks can measure occlusal force by how they appear (Figure 1) [1-3]. Moreover, it has been shown in 3 separate studies that clinicians choose forceful contacts poorly when Subjectively Interpreting articulating paper marks [4-6]. This leads to numerous occlusal adjustment errors that shorten restoration longevity, prolong patient acceptance of new restorations, cause Temporomandibular Disorder symptoms after orthodontics [7], promote fractures of implant components [8] and complicate the practice of occlusion for the clinician. A recent systematic review determined little evidence supports using traditional occlusal indicators because they measure nothing occlusal, and their use is highly subjective and inaccurate [9].
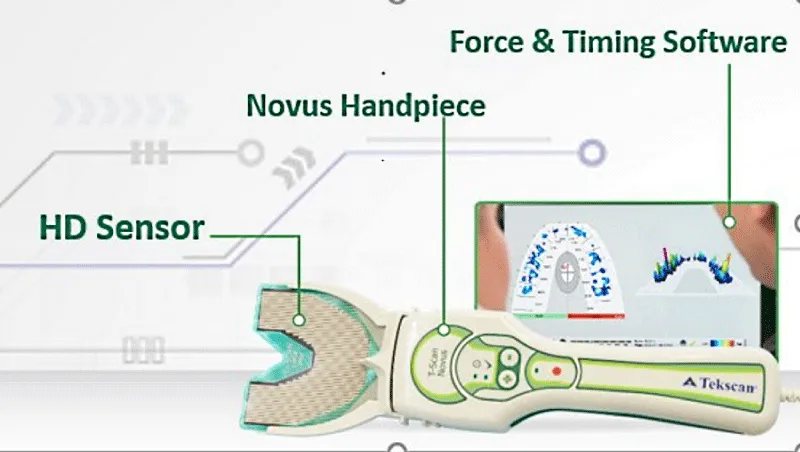
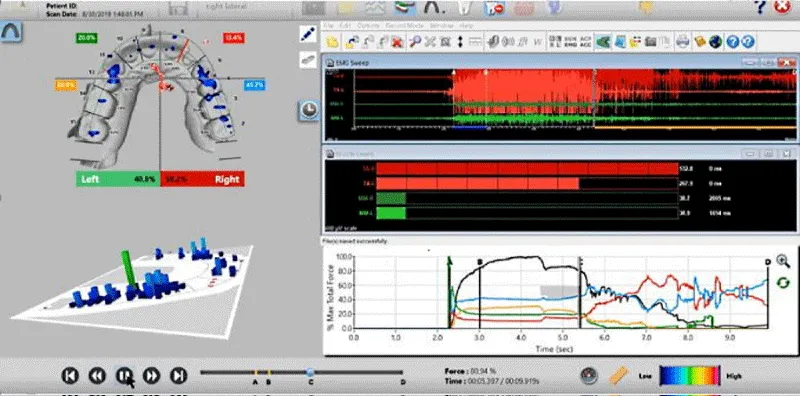
Presently, Dental Medicine is incorporating digital technologies into the Digital Workflow (intraoral scanning; CAD/CAM milling, and restorative fabrication), which improves outcomes beyond what is possible with traditional, non-digital methods. An example is employing scanning, virtual articulation, and virtual mandibular motion compared to mounting stone casts with a facebow registration and plaster and manually moving the casts on an articulator that poorly approximates human motion. Scanning and virtual articulation eliminate the spatial errors inherent in the facebow method (impression distortion, stone, and mounting plaster setting contraction, wax imprint distortion, and mechanical articulator motion), while virtual articulation closely reproduces human mandibular motion patterns. Further, the addition of digital occlusal technology with the T-Scan 10 Novus Computerized Occlusal Analysis system (Tekscan Inc. S., Boston, MA USA) to both diagnose and guide occlusal adjustments, has been shown for nearly 4 decades to improve occlusal outcomes over traditional non-digital occlusal indicators (Figure 2a) [10-19] This is because T-Scan 10 objectively measures relative occlusal forces, contact timing, and overall occlusal force distribution non-subjectively, accurately, and repeatedly [9], such that when compared to traditional occlusal indicators, that same systematic review determined that much scientific evidence supports the use of T-Scan [9,20-23].
So, how should State of the Art occlusion be practiced in the Digital Era of Dental Medicine? By employing 2 complimentary occlusal measurement technologies that quantify occlusal function. They are:
- The T-Scan 10 Novus Computerized Occlusal Analysis System (Figures 2a-c)
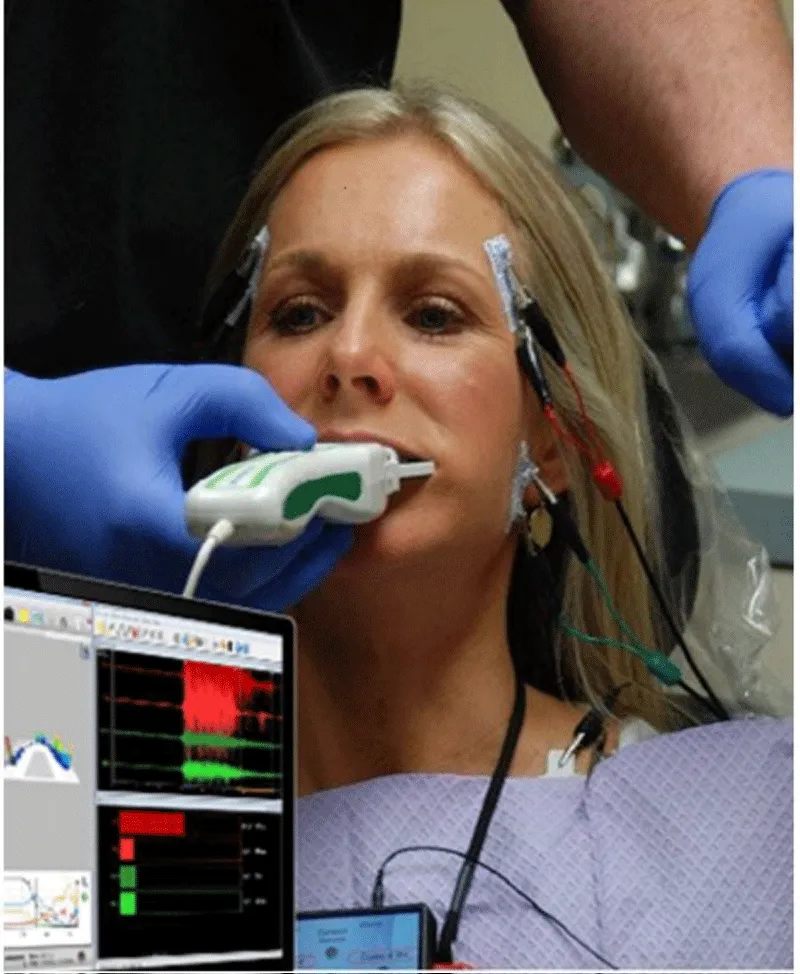
- Synchronized Surface Electromyography BioEMG III (sEMG; Bioresearch Associates, Milwaukee, WI, USA) (Figure 3).
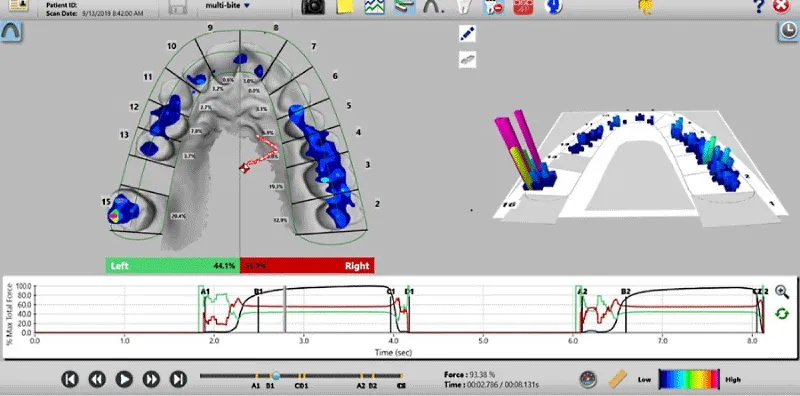
The T-Scan 10, with its 5th generation High Definition (HD) recording sensor (Novus HD, Tekscan, Inc., S. Boston, MA, USA), can record 256 relative occlusal contact force levels across elapsed time in 0.003 second-long increments. When a patient occludes upon the electronically-charged HD sensor (Figure 2b), opposing teeth make approximating contact and compress together the upper and lower sensor surfaces, which results in a change in the electronic resistance in each of the contacted 0.5 mm2 force measurers (known as sensels). These resistance changes are measured by the T-Scan 10’s hardware electronics as a change in Digital Output Voltage (DO) [24] Higher contact force produces large resistance changes and low contact force produces lesser resistance changes. The T-Scan 10 software uses a multi-colored 2 and 3-dimensional graphical desktop display (Figure 2c), to represent the variable changing occlusal forces that rise during complete intercuspation or engage frictionally during mandibular excursive movements [24] This non-subjective occlusal force distribution diagnosis can guide occlusal treatment to reach high-precision occlusal contact timing and force treatment end-points that cannot be achieved with the subjectively assessed, non-digital occlusal indicators [9,17], or with scanner occlusograms, which contain no true force measurements and solely project the geometry of occluding teeth [9,24].
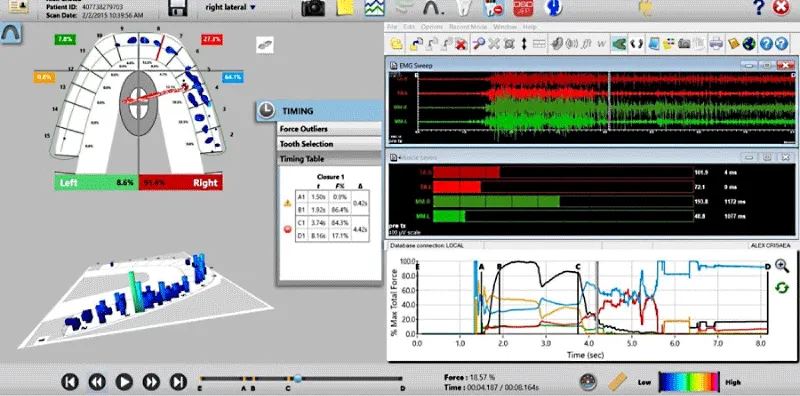
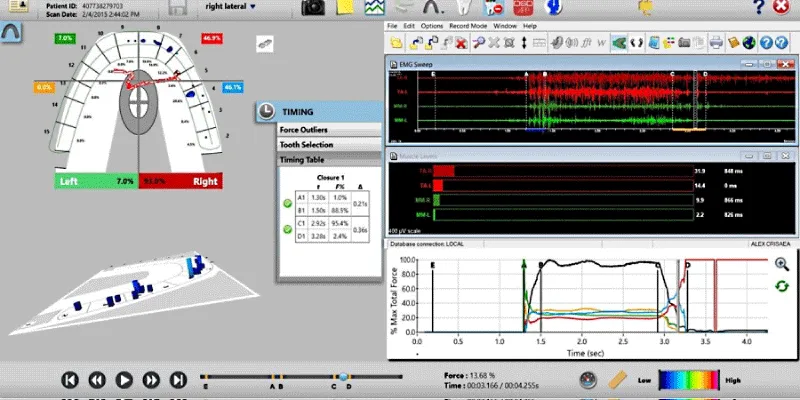
Surface Electromyography (BioEMG III) can record varying muscle contraction levels of the superficial masseter, the anterior temporalis, the anterior digastric, and the sternocleidomastoid muscles, in both healthy and dysfunctional muscles. The T-Scan 10 and the/BioEMG III when paired together have synchronized data sets [19], representing a major advance in the study of occlusal function by simultaneously recording occlusal contacts and their corresponding muscle activity response (Figures 3a,b).
When prolonged posterior occlusal contacts are present in excursions, muscular hyperactivity is also present, causing muscular ischemia from lactic acid accumulation, and the clinical appearance of muscular symptoms [10-19]. The mechanism of muscular hyper contraction is a posterior pulp and PDL mechanoreceptor mediated process, resultant from prolonged excursive opposing posterior teeth occlusal surface engagements, that directly elevate masticatory muscle activity through the unique neuroanatomy of the molar and premolar pulp/PDL fibers, which synapse with the Trigeminal Motor Nucleus [25]. Every time opposing posterior teeth contact or flex under excursive loading, masticatory muscle activity is created directly from this neural mechanism (Figure 4).
An example of using the T-Scan 10/BioEMG III to remove muscular hyperactivity by altering the time duration of excursive occlusal contacts (known as the Disclusion Time [20]) can be seen in Figures 5-7.
For many years, a female patient experienced chronic bilateral masseter tension, frequent temporal headaches, regular morning jaw soreness, daytime clenching, and nighttime bruxing, despite wearing an appliance for many years. She presented with slightly worn bilateral canine contacts (Figure 5a,b) that lacked guidance lift resulting in poor posterior disclusion.
Pretreatment articulating paper linear marks that depict the right excursion’s long Disclusion Time and frictional excursive contacts (Figure 6a) is then treated with ICAGD, based on the pretreatment right excursive T-Scan data.
Reducing the Disclusion Time is accomplished by performing the Immediate Complete Anterior Guidance Development coronoplasty (ICAGD) [10], which is a measurement-driven, excursively focused computer-guided occlusal adjustment procedure that shortens prolonged excursive occlusal surface contact to a Disclusion Time to < 0.5 seconds per excursion [10,21,24,26-28] ICAGD is performed in the maximum intercuspal position (MIP) [11] simplifying treatment as no Bimanual Manipulation to CR is employed, no jaw repositioning with splints/orthotics are needed, and no vertical dimension changes are utilized [10-19]. Shortening the Disclusion Time drastically reduces posterior teeth compression and flexure so their pulp and PDL fibers fire muscles for far less time than pre-ICAGD [10-19] Correctly performed ICAGD removes all linear contacts leaving only small points that reflect almost no “time travel” of opposing occlusal surfaces (Figure 6b). This process is repeated with the left excursion (not shown for brevity) until visual disclusion has been achieved bilaterally (Figure 6c).
Physiologic muscle activity level changes can be seen by comparing Figure 7 (the post ICAGD right excursion) to Figure 4. This muscular relaxation is why shortening the Disclusion Time with ICAGD is an effective Occluso-muscle Disorder treatment [10-19].
It is through the simultaneous measurement of the occlusion and muscles with the T-Scan 10/BioEMG III that computer-guided occlusal treatment can predictably improve Occluso-muscle Disorder symptoms [10-19] when compared to the poor therapeutic effectiveness of unmeasured and subjectively interpreted paper mark-only occlusal adjustments.
So, practicing Occlusion in the Digital Era of Dental Medicine should require the use of State of the Art occlusal measurement technologies.
Conflict of interest disclosure
The Author is a Clinical Consultant for Tekscan, Inc., but receives no compensation for sales of the product
- Carey J, Craig M, Kerstein RB, Radke J. Determining a relationship between applied occlusal load and articulation paper mark area. Open Dentistry Journal. 2007; 1: 1-7.
- Saad MN, Weiner G, Ehrenberg D, Weiner S. Effects of load and indicator type upon occlusal contact markings. J Biomed Mater Res B Appl Biomater. 2008 Apr;85(1):18-22. doi: 10.1002/jbm.b.30910. PMID: 17618516.
- Qadeer S, Kerstein R, Kim RJ, Huh JB, Shin SW. Relationship between articulation paper mark size and percentage of force measured with computerized occlusal analysis. J Adv Prosthodont. 2012 Feb;4(1):7-12. doi: 10.4047/jap.2012.4.1.7. Epub 2012 Feb 29. PMID: 22439094; PMCID: PMC3303923.
- Kerstein RB, Radke J. Clinician accuracy when subjectively interpreting articulating paper markings. Cranio. 2014 Jan;32(1):13-23. doi: 10.1179/0886963413Z.0000000001. PMID: 24660642.
- Sutter BA. A digital poll of dentists testing the accuracy of paper mark subjective interpretation. Cranio. 2018 Nov;36(6):396-403. doi: 10.1080/08869634.2017.1362786. Epub 2017 Aug 9. PMID: 28792294.
- Basson E, Kerstein RB, Radke J. Ability to Correctly Select High Force Occlusal Contacts from Articulating Paper Markings. Adv Dent Tech. 2020; 2(1): 101-10.
- Qadeer S, Abbas AA, Sarinnaphakorn L, Kerstein RB. Comparison of excursive occlusal force parameters in post-orthodontic and non-orthodontic subjects using T-Scan® III. Cranio. 2018 Jan;36(1):11-18. doi: 10.1080/08869634.2016.1259785. Epub 2016 Nov 23. PMID: 27876452.
- Sailer I, Strasding M, Valente NA, Zwahlen M, Liu S, Pjetursson BE. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic multiple-unit fixed dental prostheses. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:184-198. doi: 10.1111/clr.13277. PMID: 30328185.
- Qadeer S, Özcan M, Edelhoff D, Van Pelt H. Accuracy, Reliability and Clinical Implications of Static Compared to Quantifiable Occlusal Indicators. Eur J Prosthodont Restor Dent. 2021 Aug 31;29(3):130-141. doi: 10.1922/EJPRD_2202Qadeer12. PMID: 33508180.
- Kerstein RB, Wright NR. Electromyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: before and after treatment with immediate complete anterior guidance development. J Prosthet Dent. 1991 Nov;66(5):677-86. doi: 10.1016/0022-3913(91)90453-4. PMID: 1805009.
- Kerstein RB. Reducing chronic masseter and temporalis muscular hyperactivity with computer-guided occlusal adjustments. Compend Contin Educ Dent. 2010 Sep;31(7):530-4, 536, 538 passim. PMID: 20879206.
- Kerstein RB, Radke J. The effect of disclusion time reduction on maximal clench muscle activity levels. Cranio. 2006 Jul;24(3):156-65. doi: 10.1179/crn.2006.026. PMID: 16933455.
- Kerstein RB, Radke J. Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Cranio. 2012 Oct;30(4):243-54. doi: 10.1179/crn.2012.038. PMID: 23156965.
- Thumati P, Manwani R, Mahantshetty M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. Cranio. 2014 Oct;32(4):289-99. doi: 10.1179/2151090314Y.0000000004. Epub 2014 Apr 30. PMID: 25252768.
- Yiannios N, Kerstein RB, Radke J. Treatment of frictional dental hypersensitivity (FDH) with computer-guided occlusal adjustments. Cranio. 2017 Nov;35(6):347-357. doi: 10.1080/08869634.2016.1251692. Epub 2016 Nov 11. PMID: 27835932.
- Thumati P, Thumati RP. The effect of disocclusion time-reduction therapy to treat chronic myofascial pain: A single group interventional study with 3 year follow-up of 100 cases. J Indian Prosthodont Soc. 2016 Jul-Sep;16(3):234-41. doi: 10.4103/0972-4052.176529. PMID: 27621541; PMCID: PMC5000572.
- Thumati P. The influence of immediate complete anterior guidance development technique on subjective symptoms in Myofascial pain patients: Verified using digital analysis of occlusion (Tek-scan) for analysing occlusion: A 3 years clinical observation. J Indian Prosthodont Soc. 2015 Jul-Sep;15(3):218-23. doi: 10.4103/0972-4052.158079. PMID: 26929516; PMCID: PMC4762330.
- Thumati P, Sutter B, Kerstein RB, Yiannios N, Radke J. Changes in the Beck Depression Inventory-II Scores of TMD Subjects after Measured Occlusal Treatment. Adv Dent Technol. 2018; 1: 1-13.
- Thumati P, Poovani S, Bharathi B, Mounika A, Kerstein RB, Radke J. A Disclusion Time Reduction Randomized Controlled Occlusal Adjustment Trial. Adv Dent Technol. 2020; 2: 1-23.
- Hirano S, Okuma K, Hayakawa I. [In vitro study on accuracy and repeatability of the T-Scan II system]. Kokubyo Gakkai Zasshi. 2002 Sep;69(3):194-201. Japanese. doi: 10.5357/koubyou.69.194. PMID: 12400174.
- Kerstein RB, Lowe M, Harty M, Radke J. A force reproduction analysis of two recording sensors of a computerized occlusal analysis system. Cranio. 2006 Jan;24(1):15-24. doi: 10.1179/crn.2006.004. PMID: 16541841.
- Koos B, Godt A, Schille C, Göz G. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch. J Orofac Orthop. 2010 Nov;71(6):403-10. English, German. doi: 10.1007/s00056-010-1023-7. Epub 2010 Nov 17. PMID: 21082303.
- Andrus R, Quian F, Weir D, Schneider R, Huber L, Kerstein RB. Comparison of results of traditional occlusal adjustment technique w/ computer-aided occlusal adjustment technique. Advanced Technologies and Techniques. 2019; 1(2): 43-53.
- Anselmi R. T-Scan 10 Recording dynamics, system features, and clinician user skills required for T-Scan chairside mastery. In Handbook of Research on Clinical Applications of Computerized Occlusal Analysis in Dental Medicine; Kerstein, R.B., Ed.; IGI Global Publishers: Hershey, PA, USA. 2020; 130–224.
- Haines DE. Neuroanatomy. An atlas of structures, sections, and systems, Ed.8, Baltimore MD: Lippincott, Williams, & Wilkins. 220: 199-227.
- Kerstein RB. Combining technologies: a computerized occlusal analysis system synchronized with a computerized electromyography system. Cranio. 2004 Apr;22(2):96-109. doi: 10.1179/crn.2004.013. PMID: 15134409.
- Kerstein RB. A comparison of traditional occlusal equilibration and immediate complete anterior guidance development. The Journal of Craniomandibular Practice. 1993; 11(2): 126 -140.
- Kerstein R. Disclusion time reduction therapy with immediate complete anterior guidance development: the technique. Quintessence International. 1992; 23:735 - 747.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.







 Save to Mendeley
Save to Mendeley
