International Journal of Oral and Craniofacial Science
Oral rehabilitation of a patient with Sjögren syndrome
Merima Balić1* and Zoltan Ovari2
2Cosmodent Fogaszat, Budapest, Hungary
Cite this as
Balić M, Ovari Z (2022) Oral rehabilitation of a patient with Sjögren syndrome. Int J Oral Craniofac Sci 8(2): 020-022. DOI: 10.17352/2455-4634.000054Copyright License
© 2022 Balić M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Introduction
Sjögren syndrome (SS) is a chronic autoimmune disease characterized by inflammation of salivary and lacrymal glands, causing oral and ocular dryness [1]. The syndrome was named by Swedish ophthalmologist Henrik Sjögren, who identified it in 1933. SS prevalence ranges between 0. 5 % and 3 % and the syndrome is more likely to affect females over 40 years old, especially in menopause [2, 3]. It is a slowly progressing, non-life-threatening disease with a 10-year cumulative survival rate of over 90 % [4].
Primary SS involves only salivary and lacrymal glands and lymphocyte infiltration of these glands is a hallmark of primary SS. Secondary SS is associated with other autoimmune diseases like rheumatoid arthritis, systemic lupus erythematosus, polyarthritis nodosa, or scleroderma [5]. The diagnosis of SS is based on clinical, laboratory, imaging, and pathological criteria, as defined by the American-European consensus [6].
Xerostomia (mouth dryness) and xerophthalmia (eye dryness) are the main symptoms of Sjögren syndrome, occurring in more than 95 % of patients. Oral symptoms are mainly consequences of hyposalivation. Difficulty in mastication and dysphagia occur as a lack of saliva in softening and lubricating food. The decreased immunological and protective salivary function makes patients prone to local infections like angular cheilitis and oral candidiasis. Tongue depapillation is connected to the loss of taste sensation or stomathopyrosis (burning sensation of the oral mucosa). However, the greatest problem caused by hyposalivation is a high caries risk and with that associated tooth wear. Caries occur more easily, because of the missing buffering capacity of saliva, which leads to prolonged acidic pH that facilitates enamel deminarelaziation [7].
Therefore, the purpose of this paper is to present a contemporary approach to the treatment of a patient with Sjögren syndrome using multilayered monolithic single zirconia crowns.
Case report
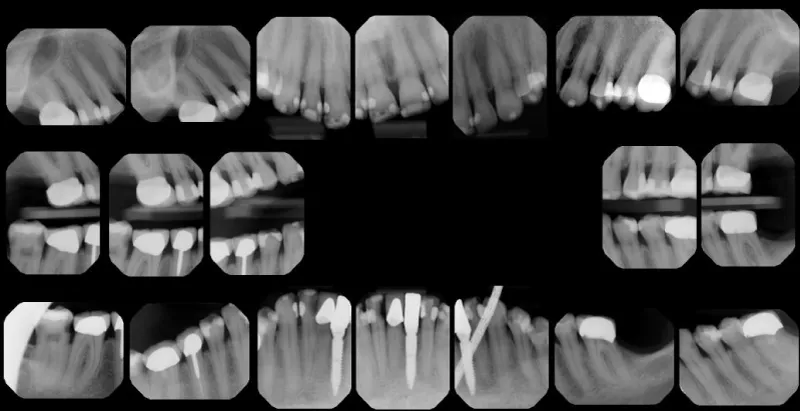
A 61-year-old woman previously diagnosed with Sjögren syndrome presented to our clinics with dissatisfaction with her smile (Figure 1). The patient signed informed consent to the publication of images and clinical information. Extraoral examination revealed xeropthalmia. Intraoral examination revealed dry oral mucosa, multiple carious lesions, and old fillings.
Occlusal analysis revealed an interocclusal distance of 5 mm, suggesting a decreased vertical dimension [8].
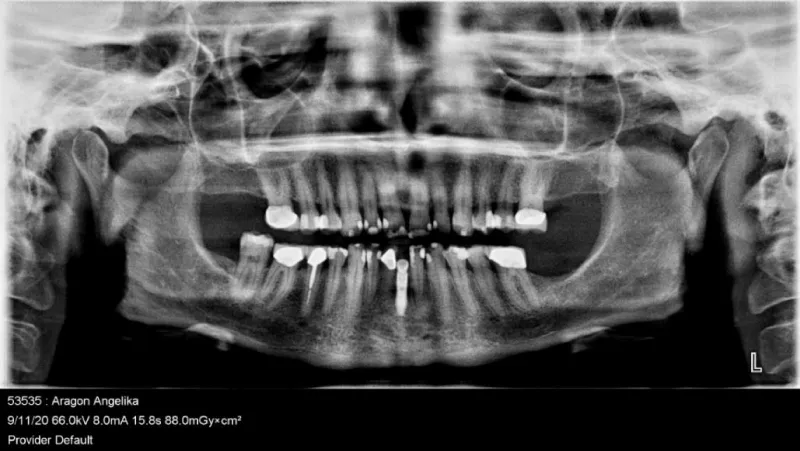
Radiographic examination confirmed the presence of primary and secondary carious lesions (Figure 2). Old fillings with marginal pigmentation needed to be changed. Tooth 47 presented with caries profunda and was planned to be extracted due to a missing antagonist. Tooth 42 presented with caries profunda and needed root canal treatment. Tooth 45 presented with defective endodontic treatment, but without translucency or symptoms. The implant crown in place of the lower left central incisor was clinically and radiologically in good condition, with no need for treatment (Figure 3). After clinical and radiographic examinations, a treatment plan including a total of 19 single zirconia crowns in both jaws was made, in order to achieve aesthetic and functional improvement.
Root canal treatment and extraction were made together with alginate impressions and bite registration for model analysis. As the extraction site did not affect the prosthodontic plan, two weeks later, the teeth were prepared with an epigingival chamfer finish line. On the same day, two-phase definitive impressions in both jaws were made using silicone impression material (Elite HD putty and light flow; Zhermack, Badia Polesine, Italy). Centric relation was registered using a light-curing hard composite jig and silicone for bite registration (Occlufast; Zhermack, Badia Polesine, Italy). The vertical dimension was determined by measuring CEJ distance between upper and lower right central incisor, with a 1,5 mm increased vertical dimension compared to habitual occlusion height.
The crowns were firstly milled in PMMA (Temp Esthetic; Harvest Dental). The next day, PMMA restorations were used for trial and evaluation of the marginal fit, occlusal/proximal contacts, esthetics, and phonetics. After intraoral adjustments, PMMA crowns were cemented provisionally (Figure 4).
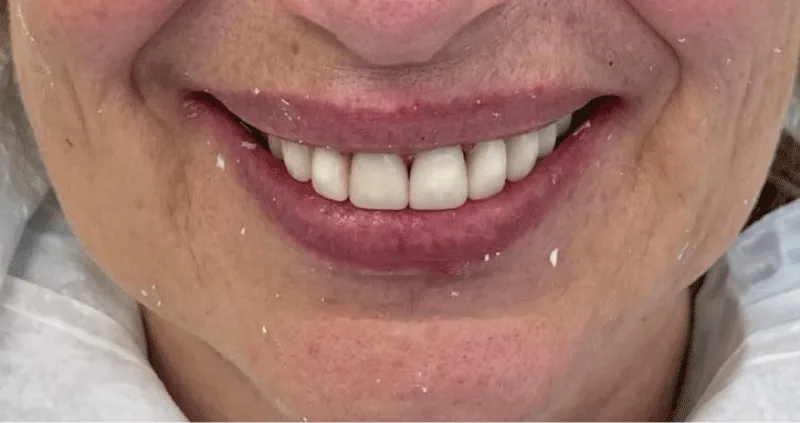
Three months later, PMMA restorations were scanned and milled from zirconia (Prettau 3 dispersive®, Zirkonzahn, South Tirol, Italy) with gradations of translucency for optimal esthetics. The definitive restorations were cemented, using a resin-modified glass ionomer cement (FujiCEM 2; GC America). The patient was very satisfied with her new smile (Figure 5). Due to a change in the vertical dimension, the occlusal guide was fabricated, and the patient was advised to use it at night. The first check-up was made one day after placing restorations, and the second one week later. Small occlusal adjustments were made on the second check where the patient also expressed her satisfaction with biting and the functional segment of rehabilitation.
Discussion
Treatment of Sjögren’s syndrome depends on the extent and severity of the clinical manifestations. For mouth dryness mouthwashes, chewing gums, and salivary substitutes are recommended. Systemic use of muscarinic agonists (pilocarpine) has been shown to increase saliva production [9]. One study reported an improvement of xerostomia with topical use of liquid pilocarpine, with fewer side effects compared to systemic use [10]. Caries prevention is achieved with fluoride toothpaste combined with fluoride gels or chewable tablets [11]. Candidiasis is treated by antifungal medications. Also, hormonal replacement therapy (estradiol) in menopause can help in a 10-20% reduction in xerostomia.
On the other hand, restorative and prosthetic treatment of a patient with SS depends on the severity of occlusal wear. In general, due to the dry mouth, mucosal atrophy, and tendency to infections, prosthodontic treatment with a tissue-supported or removable prosthesis is not recommended. Treatment consisting of crowns or fixed bridges with a canine-protected occlusion has been long ago reported, as a treatment of choice in patients with Sjogren’s syndrome [12]. In this case, the treatment included fixed restorations (single crowns), because they ensure easier cleaning and better oral hygiene. Furthermore, they provide a more esthetical and natural appearance. All ceramic or zirconia crowns may also ensure better long-term protection than composite restorations, and lower caries risk connected to hyposalivation.
To the best of our knowledge, literature and follow-up data on prosthetic treatment with ceramic crowns in SS patients is limited. However, in a case report by Fradeani, et al. [13] minimally invasive treatment approach using a lithium disilicate all-ceramic material for the esthetic rehabilitation of a patient diagnosed with SS, was described. Similar to our case, Francois Fisselier, et al. [6] reported successful treatment of a patient with SS, using multilayered monolithic zirconia restorations. Contrary to the report of Fisselier, in our case, all restorations are made as single, separate crowns. We believe that single crowns ensure better and easier oral hygiene than crowns connected to a bridge. Consequently, they may reduce the high caries risk and help maintain good periodontal health in patients with SS.
Conclusion
Sjögren syndrome is not an obstacle to a successful and predictable prosthodontic treatment. In our case, zirconia, single restorations ensured optimal restoration of function, occlusion, and esthetics in oral rehabilitation of the patient with SS.
- Sjögren H. On knowledge of keratoconjunctivitis sicca; keratitis filiformis by hypofunction of lacrimal glands. Acta Ophthalmol 1933;(suppl 2):1-151.
- Clio P, Mavragani MD, Haralampos M, Moutsopoulos MD. Sjogren Syndrome CMAJ2014; 186
- Hammitt KM, Naegeli AN, van den Broek RWM, Birt JA. Patient burden of Sjögren's: a comprehensive literature review revealing the range and heterogeneity of measures used in assessments of severity. RMD Open. 2017 Sep 17;3(2):e000443. doi: 10.1136/rmdopen-2017-000443. PMID: 28955493; PMCID: PMC5604724.
- Zandonella Callegher S, Giovannini I, Zenz S, Manfrè V, Stradner MH, Hocevar A, Gutierrez M, Quartuccio L, De Vita S, Zabotti A. Sjögren syndrome: looking forward to the future. Ther Adv Musculoskelet Dis. 2022 May 23;14:1759720X221100295. doi: 10.1177/1759720X221100295. PMID: 35634352; PMCID: PMC9131387.
- Bayetto K, Logan RM. Sjögren's syndrome: a review of aetiology, pathogenesis, diagnosis and management. Aust Dent J. 2010 Jun;55 Suppl 1:39-47. doi: 10.1111/j.1834-7819.2010.01197.x. PMID: 20553243.
- Fisselier F, Comut AA. Contemporary management and full mouth rehabilitation of a patient with Sjögren syndrome. J Prosthet Dent. 2018 Jul;120(1):5-8. doi: 10.1016/j.prosdent.2017.10.015. Epub 2017 Dec 16. PMID: 29258693.
- Pedersen AM, Bardow A, Nauntofte B. Salivary changes and dental caries as potential oral markers of autoimmune salivary gland dysfunction in primary Sjogren's syndrome. BMC Clin Pathol. 2005 Mar 1;5(1):4. doi: 10.1186/1472-6890-5-4. PMID: 15740617; PMCID: PMC554998.
- Standard SG, Lepley JB. The free-way space and its relation to the temporomandibular articulation. J Prosthet Dent 1955;5:20-32.
- Kassan SS, Moutsopoulos HM. Clinical manifestations and early diagnosis of Sjögren syndrome. Arch Intern Med. 2004 Jun 28;164(12):1275-84. doi: 10.1001/archinte.164.12.1275. PMID: 15226160.
- Watanabe M, Yamada C, Komagata Y, Kikuchi H, Hosono H, Itagaki F. New low-dose liquid pilocarpine formulation for treating dry mouth in Sjögren's syndrome: clinical efficacy, symptom relief, and improvement in quality of life. J Pharm Health Care Sci. 2018 Mar 1;4:4. doi: 10.1186/s40780-018-0099-x. PMID: 29507747; PMCID: PMC5831212.
- Jonsson MV, Delalue N. Marthinussen. MC Oral and dental manifestations of Sjogren’s syndrome: current approaches to diagnostics and therapy. Sjogren’s syndrome. Berlin: Springer. 2012; 221-42.
- Barker BF, Moffitt MW, Johnson JK. Sjögren's syndrome: diagnosis and dental treatment. J Prosthet Dent. 1978 May;39(5):536-8. doi: 10.1016/s0022-3913(78)80189-9. PMID: 274547.
- Fradeani M, Barducci G, Bacherini L, Brennan M. Esthetic rehabilitation of a severely worn dentition with minimally invasive prosthetic procedures (MIPP). Int J Periodontics Restorative Dent. 2012 Apr;32(2):135-47. PMID: 22292142.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
