Journal of Dental Problems and Solutions
Prosthodontic Aspects of Splinting the Mandibular Anterior Teeth by Fiber Reinforced Composites
Miroslav Hrelja1, Mirko Laškarin2, Samir Čimić3, Sonja Kraljević3, Nikša Dulčić3 and Tomislav Badel3*
1Dental office, Dugo Selo, Croatia
2Health Center Šibenik, Šibenik, Croatia
3Department of Removable Prosthodontics, School of Dental Medicine, University of Zagreb, Zagreb, Croatia
Cite this as
Hrelja M, Laškarin M, Čimić S, Kraljević S, Dulčić N, Badel T. Prosthodontic Aspects of Splinting the Mandibular Anterior Teeth by Fiber Reinforced Composites. J Dent Probl Solut. 2025;12(1):004-008. Available from: 10.17352/2394-8418.000131Copyright License
© 2025 Hrelja M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.This paper deals with the advantages and the procedures used in resolving prosthodontic problems in cases of partial edentulousness by using the remaining anterior mandibular teeth. The clinical report presents atraumatic splinting of mandibular teeth for prosthodontic and periodontal purposes with a review of changed occlusal conditions in a clinical case of prosthodontic treatments of partial edentulousness. The splints with fewer teeth involved (two to four) showed greater durability than those with a large number of teeth. The advantages of using a Fiber Reinforced Composite (FRC) splint were analyzed with the aim of noninvasive bonding of the remaining periodontopathic teeth. By splinting the mandibular anterior teeth (Kennedy class I), a FRC splint increases their functional value (masticatory, esthetic and phonatory) and the ability of static and dynamic group loading (intermaxillary and occlusal relations). The durability of such splints is estimated on the basis of stability between the enamel and FRC and the stability of the FRC surface and total mobility of teeth stabilized by such a splint. FRC splints are easy to repair. However, the level of oral hygiene also has a significant effect on the success of FRC splint treatment.
Introduction
Partial edentulousness of the mandible according to Kennedy Class I can be primarily treated by direct tight splinting of teeth as a block using fixed prosthodontic or conservative procedures [1-3].
Mutually protected occlusion (canine/anterior teeth guidance) is according to contemporary opinion an optimal occlusal relationship between fully or at least partially dentulous jaws which preserves teeth, the supporting structures, the structures of the Temporomandibular Joint (TMJ) and masticatory muscles from functional impairments [4-6].
By losing the lateral teeth (posterior occlusal collapse), the mechanism of mutually protected occlusion stops functioning as a whole. Preserving the remaining lower anterior teeth depends on their periodontal status and thereby it is also relevant for [7-10]:
- Preserving the vertical and horizontal occlusal dimensions (static occlusion) – temporarily during the preparatory treatment procedures,
- Functioning of excursive mandibular movements (dynamic occlusion): anterior guidance on protrusion and canine guidance on lateral movements,
- Maintaining the neuromuscular patterns of functional movements before they are disturbed by loss of teeth and its compensatory mechanisms, and the self-protecting mechanisms may lead to adverse outcomes such as occlusal trauma.
Fiber Reinforced Composite (FRC) splint
Primary or direct splinting of adjoining teeth into a “block” can be achieved conservatively by adhesive techniques of fiber reinforced composite wherein the periodontium of all splinted teeth in a row is loaded at the same time. Fixed (primary) splinting of adjacent mandibular anterior teeth can be achieved by FRC for dental purposes: the adhesive technique creates a splint which can bind the remaining teeth extracoronally and conservatively. The FRC splint which is used to bind the remaining mandibular anterior teeth is the obvious biocompatible, cost-effective, and esthetically acceptable system for the patient while simultaneously being durable enough from the periodontal point of view [11].
The adhesive technique of stabilizing an extracoronal splint is based on attaching the FRC structure onto the etched enamel. The bond between the FRC splint which sits on the lingual and partially on interdental surfaces of the tooth is achieved by the microroughness of the enamel and the use of composite adhesives [12,13].
FRC for dental use are made of an organic (resinous) matrix (bisphenol-A-glycidyl methacrylate, bisGMA, polymethyl methacrylate) inorganic filler (micro or nano sized glass crystals, ceramics, zirconium, etc.) and are additionally reinforced by a fibrous structure which can efficiently transfer and distribute masticatory loads. Due to its woven cross-linked structure into 2-, 3- and 4-mm threads, the polyethylene fiber prevents the composite structure from fracturing and makes the FRCs long-lasting. The material is well adjusted to the dental surfaces it has to bind together. The intraoral constructions (splint, bridge) fabricated in this way are durable, easy to modify and have good esthetic features [14-18].
The aim of this paper is to show atraumatic splinting of lower teeth for prosthodontic and periodontal purposes with a review of changed occlusal conditions in a clinical case of prosthodontic treatments of partial edentulousness. The adhesive technique of bonding the fiber reinforced composites was used with Removable Partial Denture (RPD). The justification for using the atraumatic adhesive splinting of teeth has been confirmed by reviewing an example from practice.
Case description
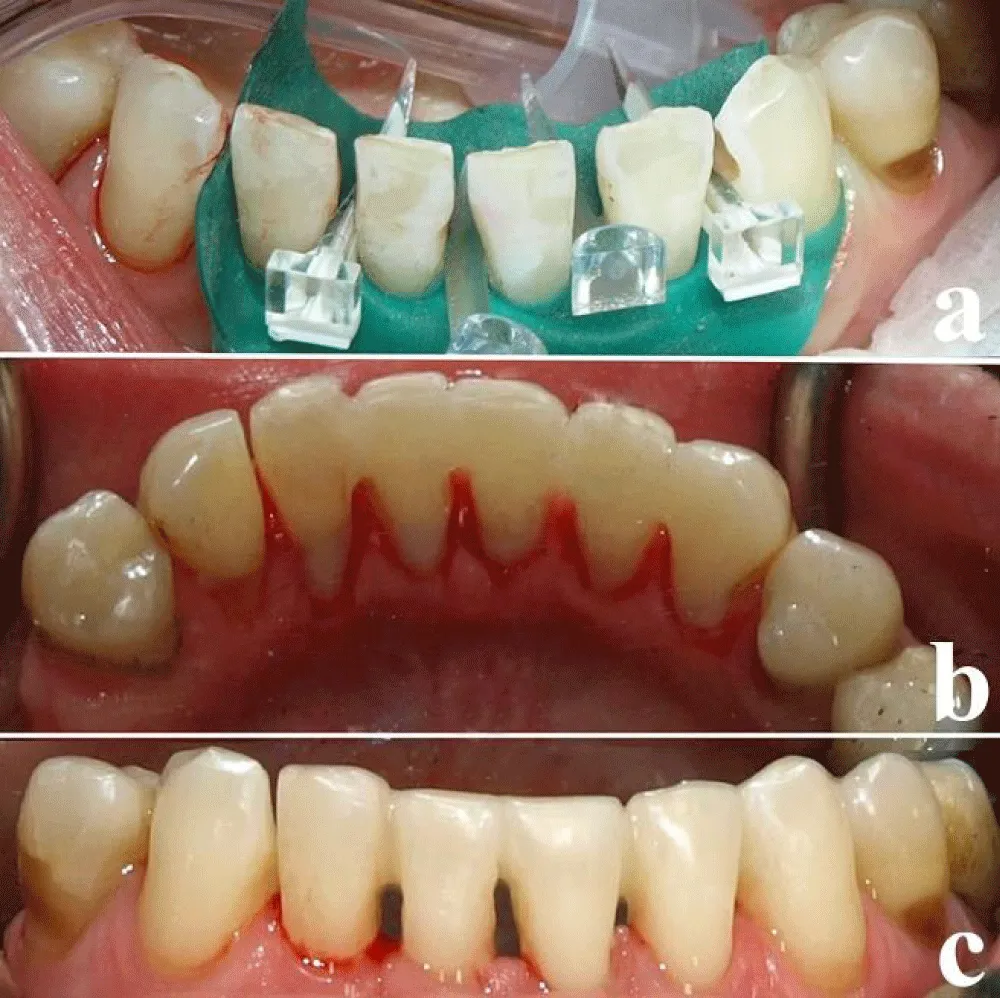
A female patient, aged 50, came to the clinic due to an untreated condition of several missing distal teeth in the mandible. A fixed-prosthodontic treatment by a semicircular bridge in the upper jaw was carried out flawlessly 2 years ago (Figure 1a).
Primary splinting
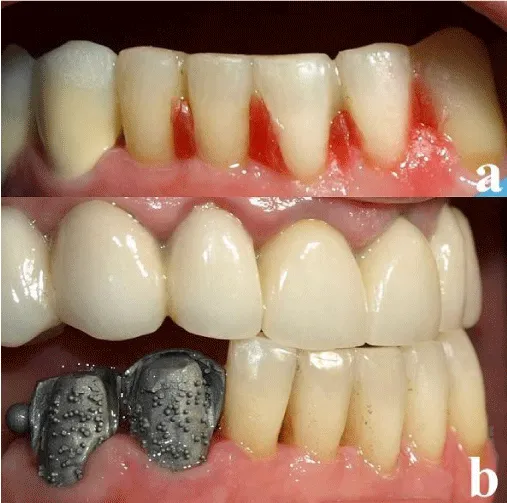
After analyzing the panoramic radiograph and the study models, a periodontal-prosthodontic plan which included splinting the anterior teeth using an FRC splint (Ribbond, Seattle, WA, USD) was made. The first step was the initial periodontal treatment including the removal of dental plaque and soft deposits by using the ultrasonic cleaning devices and abrasion by sodium bicarbonate granules (Figure 1b). After that, mandibular anterior teeth from 33 to 43 were splinted using an adhesive FRC technique (Figure 2).
Prosthodontic treatment
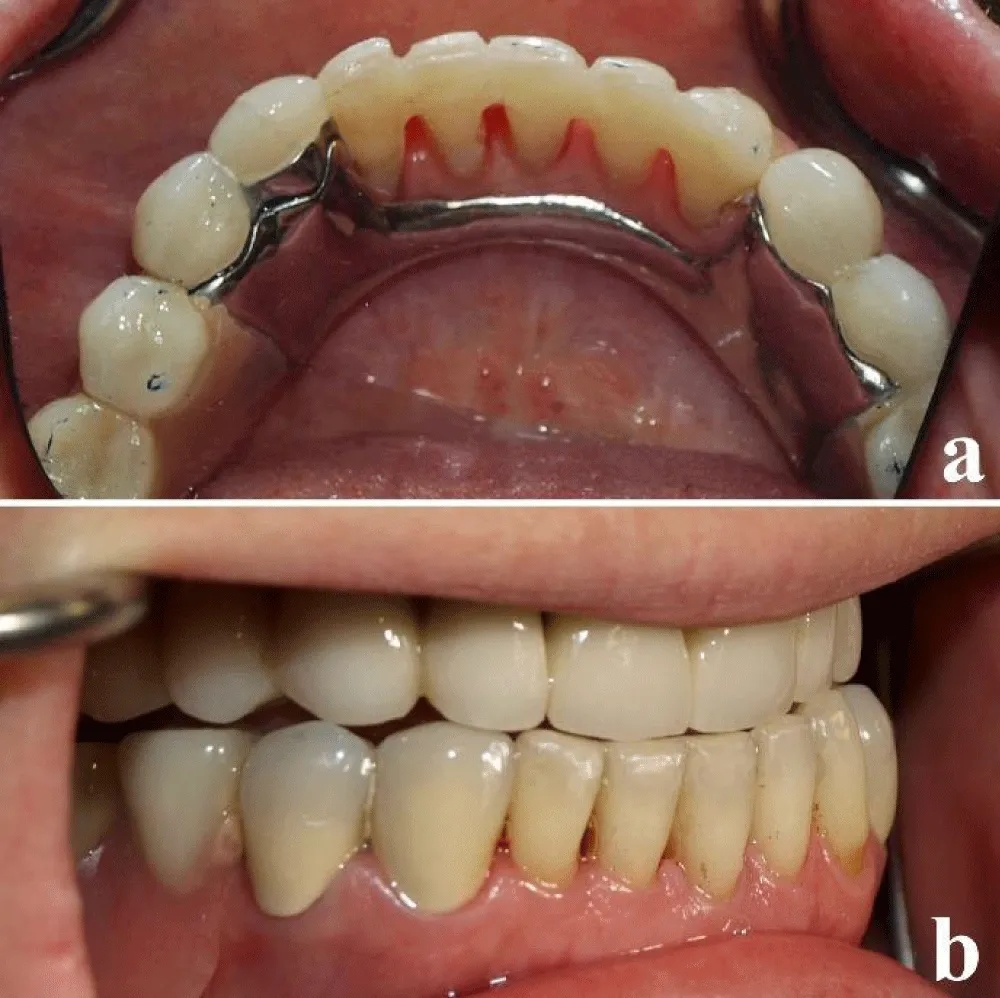
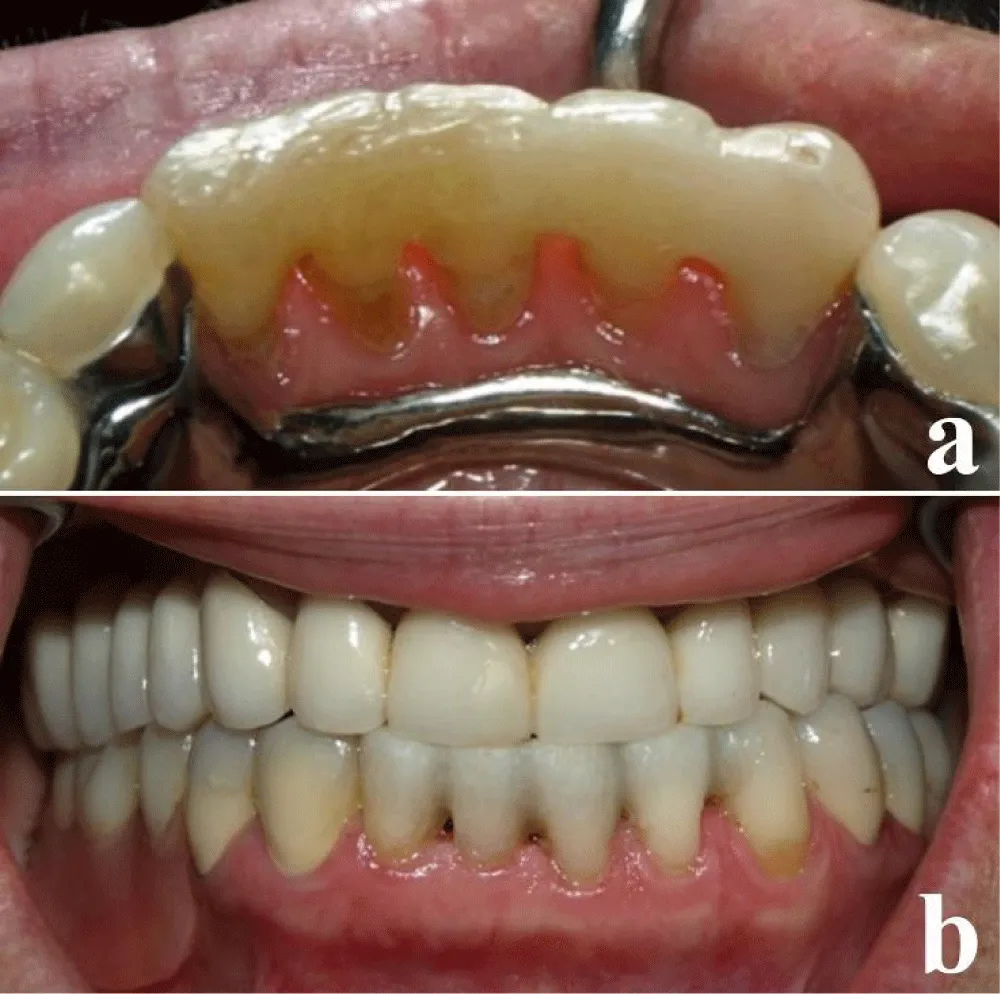
Further prosthodontic procedures indicate the taking of final impressions. The interdental spaces should be temporarily blocked out with wax before taking the impression due to periodontopathic anterior teeth with preserved contact points. In this way, the hardened impression does not get damaged when the spoon is extracted from the mouth (Figure 3a). The teeth chosen for retention of the RPD are splinted into pairs of crowns (bilaterally) in order to sustain the extracoronal load carried by the esthetic extracoronal articular attachment. In this way, the splinted teeth together with the crowned teeth maintain the vertical relation and participate in anterior guidance during mandibular movements (Figure 3b). Regarding crowns, it is important to select an esthetic layer with good tribological properties (adaptability and elasticity) to which they will be exposed during their functioning (such as the micro-filled LC composite Signum, Heraeus-Kulzer, Germany). Since the masticatory center is located on the extension base of the denture, the need arises to make an optimal selection of the replacement teeth (for example, the hybrid composite-acrylate teeth (Novo.Lign, Bredent, Germany). To achieve maximum dental loads, the extracoronal attachment-retained RPD is planned with the lingual base of the stabilizing element on the crowns (Figure 4a). Finally, RPD with crowns outside of the mouth and with invisible retention and stabilization elements. A combination of prosthodontic appliance with FRC preserved natural anterior guidance on anterior teeth (Figure 4b). Regular check-ups and hygienic maintenance of the FRC splint are inevitable prerequisites of treatment success.
Follow-up
After five years of wear, a crack in the composite filling of tooth 33 occurred within the splint and the polyethylene mesh was exposed (Figure 5a). The damage of the splint was repaired using an adhesive low viscosity flow composite method (Figure 5b).
Ten years after the first splint application, the mesh broke in one place. However, the preserved physiological mobility of mandibular anterior teeth made it possible to fabricate another splint after 10 years (Figure 6a). At the same time, the prosthesis retention was improved by replacing the matrix attachments. Vertical relation and habitual occlusion stayed unchanged throughout the whole period of time (Figure 6b).
Discussion
One part of the load is taken over by the remaining anterior teeth, another part by the articular surfaces of the TMJ as well as by masticatory muscles and the tongue. Due to the lack of distal support (distal tooth loss), the force of the masticatory muscles is directed to the anterior teeth, whereas contact is established in maximum intercuspation between anterior teeth. A disorder in the distribution of masticatory forces load is usually imbalanced, crosses the threshold of physiological structure loading and, in time, causes biomechanical damages: abrasions, abfractions, tooth mobility, loose teeth, etc. By splinting the lower anterior teeth (Kennedy class I and II/1), an FRC splint increases their functional value (masticatory, esthetic and phonatory) and the ability of static and dynamic group loading (intermandibular and occlusal relations). Periodontal prophylaxis has become easier compared to the conventional fixed-prosthodontic solutions. In a combination work, the FRC splint participates in retention and stabilizing of the partial denture with mainly dental transfer of masticatory forces onto the osseous foundation [14,19,20].
Enamel bonding necessary for fabrication of the FRC splint is based on enamel microroughness which is achieved by etching without significant preparation which minimizes or excludes the need for local anesthetics. Because it is painless, this method is easily applicable in patients with weakened general health and contraindications for local anesthetics and there are also no local complications caused by tooth preparation (pain, pulpitis, pulp necrosis, crown fracture, etc.) [15,19,21].
During the interim phase of prosthodontic treatment, the FRC splint helps to maintain the vertical relations of occlusion that are needed during denture fabrication to replace the lost teeth in lateral segments. By this means, the splinted and immobilized lower anterior teeth perform anterior guidance [8]. In such a case, the existing occlusal relations are accepted – conformative approach [22]. However, in prosthodontics, the indications for fabrication of a mandibular anterior splint are narrowed down with regard to conventional fixed-prosthodontic binding of teeth. When fabricating a series of fixed prosthodontic crowns on anterior teeth which also include a partial denture, it is necessary to change, that is, rearrange the occlusal relations (reorganization approach) [23-25].
Moderate tooth mobility should not preclude their inclusion in the prosthodontic plan from a prosthodontic occlusal scheme of anterior guidance on protrusive and laterotrusive mandibular movements [24,25]. If the existing intermaxillary relations are not changed (confirmation approach), the goal is to preserve and stabilize the existing anterior dentition. In this way, the patterns of neuromuscular occlusion are not altered and the entire prosthodontic treatment is better suited to the patient [26].
The prophylaxis of the periodontium has been made easier compared to the conventional fixed-prosthodontic solutions. In combination work, the FRC splint participates in retention and stabilizing of the RPD with mainly dental transfer of masticatory forces onto the osseous foundation [21,26]. Also, splinting the teeth by a fixed-prosthodontic appliance is considered to be a lengthy and expensive solution which demands more time and collaboration with the laboratory and it is essentially an invasive method of splinting the teeth by crowns which leads to the conservative method of using the FRC splint as the method of choice. The conservative adhesive splint (FRC splint) can be fabricated in one visit to the clinic at significantly lesser costs. In fact, this atraumatic procedure is carried out without any need for anesthetics in just one session; it is cost-effective and it has very predictable results [23-25,27]. Good hygiene and regular checkups of the periodontal status and occlusal relations should prevent unfavorable outcomes such as inflammation and loosening of the whole block of splinted teeth with substantial alveolar bone resorption. Dental status and tooth loss in women older than 45 years are not related to osteoporosis [28,29].
As seen from our own practical experience, in all of the 55 cases, the FRC (Ribbond, Seattle, WA, USD) splint did not last less than three years. If the ungluing (weakened adhesion) of the FRC splint occurs after more than five years, the adhesive bonding procedure should be repeated or a new prosthodontic plan should be made [30,31]. FRC splint failure can be the result of irregular wearing of the partial denture when the loss of distal support causes overloading of anterior teeth (secondary occlusal trauma relapse).
In conclusion, FRC-technology is useful for a large number of patients who need splinting of the mandibular anterior teeth in order to reduce the effects of increased mobility.
Clinical Significance
FRC is a non-invasive, completely atraumatic procedure which increases the functional capacity of a group of teeth with moderately advanced periodontal disease. In the treatment plan where without altering occlusal and intermaxillary relationships (conformative approach), the FRC splint serves as a viable alternative to traditional fixed prosthodontic splinting of teeth. In the clinical case described, attachment-retained RPD and the splinting of teeth (re-organized approach) represent a integrates both esthetic and functional benefits, particularly in preserving the continuity of physiological occlusion on anterior teeth and intermaxillary relationships.
In memoriam: Prof. Krešimir Kraljević, PhD (1935–2024).
Ethical approval
This clinical report was approved by the Ethics Committee of the School of Dental Medicine of the University of Zagreb as part of the PhD specialist thesis by Hrelja M.: Prosthodontic aspects of splinting the mandibular anterior teeth by fiber reinforced composites; and which was defended in 2022.
- Dommisch H, Walter C, Difloe-Geisert JC, Gintaute A, Jepsen S, Zitzmann NU. Efficacy of tooth splinting and occlusal adjustment in patients with periodontitis exhibiting masticatory dysfunction: a systematic review. J Clin Periodontol. 2022;49 Suppl 24:149–66. Available from: https://doi.org/10.1111/jcpe.13563
- Oki K, Ogino Y, Tsukiyama Y, Yamasaki Y, Koyano K. The impacts of prosthetic interventions on mastication predominance in Kennedy Class II patients. J Prosthodont Res. 2021;65:327–31. Available from: https://doi.org/10.2186/jpr.jpr_d_20_00055
- Jung TW, Yi YJ. Clinical outcomes of posterior implants with surveyed crowns for implant-assisted removable partial dentures: a retrospective study. Int J Oral Maxillofac Implants. 2023;38:53–61. Available from: https://doi.org/10.11607/jomi.9761
- Amin K, Vere J, Thanabalan N, Elmougy A. Occlusal concepts and considerations in fixed prosthodontics. Prim Dent J. 2019;8:20–7. Available from: https://doi.org/10.1308/205016819827601545
- Goldstein G, Goodacre C, Taylor T. Occlusal schemes for implant restorations: best evidence consensus statement. J Prosthodont. 2021;30(S1):84–90. Available from: https://doi.org/10.1111/jopr.13319
- Badel T, Pandurić J, Kraljević S, Dulčić N. Checking the occlusal relationships of complete dentures via a remount procedure. Int J Periodontics Restorative Dent. 2007;27:181–92. Available from: https://pubmed.ncbi.nlm.nih.gov/17514890/
- Hassall D. Centric relation and increasing the occlusal vertical dimension: concepts and clinical techniques - part one. Br Dent J. 2021;230:17–22. Available from: https://doi.org/10.1038/s41415-020-2502-x
- Goodacre CJ, Goodacre BJ. What occlusal scheme should be used with removable partial dentures? J Prosthodont. 2021;30(S1):78–83. Available from: https://doi.org/10.1111/jopr.13313
- Utz K-H, Lückerath W, Schwarting P, Noethlichs W, Büttner R, Gruner M, et al. Centric relation, maximal intercuspal position, and their practical implications. J Craniomand Func. 2021;13:185–202. Available from: https://www.quintessence-publishing.com/gbr/en/article/1942895/journal-of-craniomandibular-function/2021/03/centric-relation-maximal-intercuspal-position-and-their-practical-implications
- Badel T, Keros J, Šegović S, Komar D. Clinical and tribological view on tooth wear. Acta Stomatol Croat. 2007;41:355–65. Available from: https://hrcak.srce.hr/clanak/28409
- Kathariya R, Devanoorkar A, Golani R, Shetty N, Vallakatla V, Bhat MY. To splint or not to splint: the current status of periodontal splinting. J Int Acad Periodontol. 2016;18:45–56. Available from: https://pubmed.ncbi.nlm.nih.gov/27128157/
- Gupta A, Alifui-Segbaya F, Hasanov S, White AR, Ahmed KE, Love RM, et al. Material extrusion of thermoplastic acrylic for intraoral devices: technical feasibility and evaluation. J Mech Behav Biomed Mater. 2023;143:105950. Available from: https://doi.org/10.1016/j.jmbbm.2023.105950
- Heo G, Lee EH, Kim JW, Cho KM, Park SH. Fiber-reinforced composite resin bridges: an alternative method to treat root-fractured teeth. Restor Dent Endod. 2019;45:e8. Available from: https://doi.org/10.5395/rde.2020.45.e8
- Mangoush E, Garoushi S, Vallittu PK, Lassila L. Influence of short fiber-reinforced composites on fracture resistance of single-structure restorations. Eur J Prosthodont Restor Dent. 2020;28:189–98. Available from: https://doi.org/10.1922/ejprd_2075mangoush10
- Bhochhibhoya A, Guragain M, Gupta SP, Dahal S, Goel K. The association of age, gender, and reason of tooth loss with patterns of partial edentulism among patients reporting to a dental teaching hospital. Int J Prosthodont Restor Dent. 2023;13:17–21. Available from: https://www.ijoprd.com/doi/IJOPRD/pdf/10.5005/jp-journals-10019-1402
- Klarić N, Macan M, Par M, Tarle Z, Marović D. Effect of rapid polymerization on water sorption and solubility of bulk-fill composites. Acta Stomatol Croat. 2022;56:235–45. Available from: https://doi.org/10.15644/asc56/3/2
- Salem MN, Hassanein OE, El Kassas DW, Shaalan OO. Twelve-month clinical evaluation of fiber-reinforced bulk fill resin composite versus incremental packing of nanohybrid resin composite in restoration of deep proximal lesions of permanent molars: a randomized controlled trial. Acta Stomatol Croat. 2022;56:267–80. Available from: https://doi.org/10.15644/asc56/3/5
- Kraljević M, Šegović S, Badel T, Simeon P. Periapical status of endodontically treated teeth in relation to the quality of the coronal restoration. Acta Stomatol Croat. 2005;39:387–98. Available from: https://doi.org/10.1111/j.1365-2591.1995.tb00150.x
- Patnana AK, Vanga NRV, Vabbalareddy R, Chandrabhatla SK. Evaluating the fracture resistance of fiber reinforced composite restorations: an in vitro analysis. Indian J Dent Res. 2020;31:138–44. Available from: https://doi.org/10.4103/ijdr.ijdr_465_18
- Walter MH, Marré B, Dreyhaupt J, Heydecke G, Rauch A, Mundt T, et al. Rehabilitation of shortened dental arches: a fifteen-year randomised trial. J Oral Rehabil. 2021;48:738–44. Available from: https://doi.org/10.1111/joor.13167
- Jafarnia S, Valanezhad A, Shahabi S, Abe S, Watanabe I. Physical and mechanical characteristics of short fiber-reinforced resin composite in comparison with bulk-fill composites. J Oral Sci. 2021;63:148–51. Available from: https://doi.org/10.2334/josnusd.20-0436
- Davies S. Conformative, re-organized or unorganized? Dent Update. 2004;31:334–45. Available from: https://doi.org/10.12968/denu.2004.31.6.334
- Hassall D. Centric relation and increasing the occlusal vertical dimension: concepts and clinical techniques - part two. Br Dent J. 2021;230:83–9. Available from: https://doi.org/10.1038/s41415-020-2593-4
- Horga D, Badel T, Liker M, Vidović A. The influence of dental prostheses on the production of fricatives [in Croatian]. Croat Rev Rehabil Res. 2013;49(Suppl):37–49. Available from: https://www.researchgate.net/publication/287713639_The_influence_of_dental_prostheses_on_the_production_of_fricatives
- Badel T, Simonić-Kocijan S, Lajnert V, Dulčić N, Zadravec D. Michigan splint and treatment of temporomandibular joint – review of literature. Med Flum. 2013;49:112–20. Available from: https://www.researchgate.net/publication/260479563_Michigan_splint_and_treatment_of_temporomandibular_joint
- Zhang Y, Kang N, Xue F, Duan J, Chen F, Cai Y, et al. Survival of nonsurgically splinted mandibular anterior teeth during supportive maintenance care in periodontitis patients. J Dent Sci. 2023;18:229–36. Available from: https://doi.org/10.1016/j.jds.2022.05.025
- Tavangar MS, Aghaei F, Nowrouzi M. Reconstruction of natural smile and splinting with natural tooth pontic fiber-reinforced composite bridge. Case Rep Dent. 2022;2022:9974197. Available from: https://doi.org/10.1155/2022/9974197
- Savić Pavičin I, Sipina M, Badel T, Jukić T. The impact of osteoporosis on dental health in women older than 45 years. Acta Stomatol Croat. 2013;47:329–35. Available from: http://dx.doi.org/10.15644/asc47/4/5
- Sonnenschein SK, Ciardo A, Kilian S, Ziegler P, Ruetters M, Spindler M, et al. The impact of splinting timepoint of mobile mandibular incisors on the outcome of periodontal treatment—preliminary observations from a randomized clinical trial. Clin Oral Investig. 2022;26:921–30. Available from: https://doi.org/10.1007/s00784-021-04075-4
- Hrelja M, Badel T. Prosthodontic aspects of splinting the lower anterior teeth by fiber reinforced composites (FRC). In: Klaric Sever E, editor. Book of abstracts. 7th International Congress of the School of Dental Medicine University of Zagreb; 2021 May 21–22; Rovinj. Acta Stomatol Croat. 2021;55:215.
- Perrin P, Meyer-Lueckel H, Wierichs RJ. Longevity of immediate rehabilitation with direct fiber reinforced composite fixed partial dentures after up to 9 years. J Dent. 2020;100:103438. Available from: https://doi.org/10.1016/j.jdent.2020.103438
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
