Journal of Dental Problems and Solutions
Maxillary unilateral parastyle: An Orthodontist’s Conundrum
Abirami Ramesh1*, Priyanka Madhavan2, Vivek Amin3 and Jaya Ramesh4
2Post- Graduate Student, Department of Oral Pathology and Microbiology, Yenepoya Dental College, Mangalore, Karnataka, India
2Professor, Department of Orthodontics and Dentofacial Orthopedics, Yenepoya Dental College, Mangalore, Karnataka, India
4Senior Resident, Department of ENT, Kanachur Institute of Medical Sciences, Mangalore, Karnataka, India
Cite this as
Ramesh A, Madhavan P, Amin V, Ramesh J (2021) Maxillary unilateral parastyle: An Orthodontist’s Conundrum. J Dent Probl Solut 8(2): 057-059. DOI: 10.17352/2394-8418.000106The developmental anomalies can be in the form of mild alteration in shape of crown or root such as development of an extra supernumerary cusp in both primary and permanent dentition. Such developmental disturbances are rare in permanent dentition. Parastyle is one common form of accessory cusp of permanent mandibular molar. Though its presence is not an alarming condition, it is of great importance in medicolegal cases. We herein report a case of parastyle on permanent maxillary second molar, its development, classification, histopathological appearance and its clinical implications.
Introduction
Development of dentition is a cascade of events that take place due to the interaction of ectodermally derived oral epithelium and neural crest derived mesenchyme. Interference in any one of these events in tooth development leads to a developmental disturbance. The developmental anomalies can be in the form of mild alteration in shape of crown or root such as development of an extra supernumerary cusp in both primary and permanent dentition. The dental trait that are rarely encountered includes parastyle, protostylid, entoconulid and metaconulid which are anatomical variations [1].
Parastyle is a morphological anomaly and presents with a supernumerary cusp, usually found in association with buccal surface of maxillary molars on their mesial aspect. Parastyle is also known as paramolar tubercle or Bolk’s cusp in literature [2]. The presence of parastyle may not always be alarming but can also cause complications such as dental caries, sensitivity in the cusp with pulp extension due to attrition and can also cause devitalisation due to fracture. These morphological alterations are of great significance in medicolegal cases [3].
The purpose of this case report is to focus on uncommon dental trait, parastyle in permanent dentition and its management.
Case report
A 21-year-old male patient reported to the Department of orthodontics and Dentofacial orthopedics with the chief complaint of forwardly placed upper front teeth.
On extra oral examination, patient had convex profile, obtuse nasolabial angle, deep mentolabial sulcus and incompetent lips.
On intra oral examination, the patient presented with class II molar relationship both the sides, class II canine relationship both the sides, proclined upper anteriors, mild lower anterior crowding, overjet of 10mm, upper midline shifted to left side by 3mm, lower midline shifted to left side by 2mm and missing 37. Accessory cusp was noted in 17 on the buccal side which is parastyle of type 6 (Figure 1).
Discussion
Accessory or supernumerary cusp is an extra cusp associated with the tooth that is occasionally seen clinically. Among primates, certain accessory cusp has peculiar and limited distribution. One among the peculiar and rare anomaly is the parastyle, derived from the anterior portion of buccal cingulum of the molars [4].
First description on Parastyle was given by Dahlberg who reported an extra cusp on primary maxillary molar on Eskimo skull in 1950 [5]. Parastyle was then termed as “upper paramolar complex” by Kustaloghi [6]. Paramolar tubercle/parastyle vary with shape and size ranging from a small eminence on the outer surface to a well-developed lobulated cusp. Pulp may or may not always be present in the tubercle. Study has reported that the presence of parastyle is more common in Indian population [7].
Classification
Bolk, et al. classified the superstructure into two types as follows:
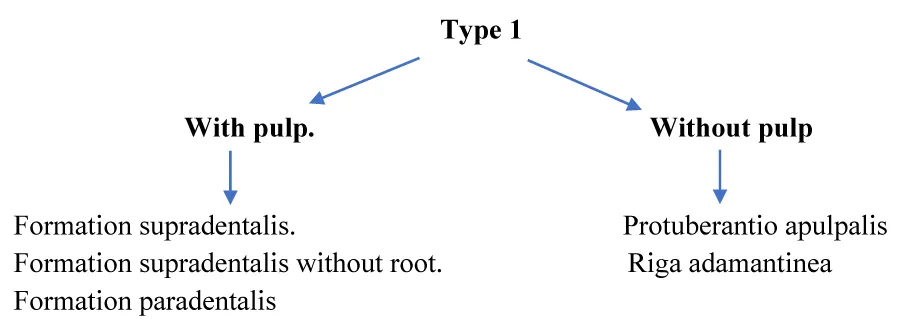
Type 1: Structure of enamel and dentin with or without the presence of pulp chamber and canal.
Type 2: Enamel prominence / overgrowth devoid of dentin and pulp.
Type 1 superstructure is further classified based on the presence or absence of pulp (Flowchart 1) [8].
The varied clinical presentation of a parastyle is best described by the scoring scale developed by Joseph F Katich and Turner (Table 1) [9].
Development
Early bell stage marks the beginning of dental cusp formation. Activators and inhibitors are produced from the proliferating inner enamel epithelium which aids in deposition of matrix from the cusp apex to the neck of the crown starting from enamel knot. Any alteration in the early bell stage may cause the formation of supernumerary cusp. Overactivity of PAX and MSX gene in dental lamina leads to abnormal shape of teeth. Mutations in Eda and Edar can also cause formation of mishappen tooth. Eda A1 over expression also causes extra cusp formation [10,11].
Histopathological appearance
The microscopic picture shows the presence of surface aprismatic enamel. The aprismatic enamel includes stunted enamel prisms in the parastyle pits, which is because of the loss of tomes’ process due to slow decline in the activity of ameloblast during amelogenesis. The enamel thickness at the pit is irregular and wrinkled with few pits of tomes’ process and presence of irregular spherical calcoglobules are also evident [12].
Clinical implications
Clinical problems observed with parastyle cases include attrition, compromised esthetics, occlusal interference, accidental cusp fracture, temporomandibular joint pain, displacement of the affected tooth, periodontal problems because of excessive occlusal force, misinterpretation of radiographs of taloned teeth before eruption and caries susceptibility because of deep developmental grooves associated with accessory cusp [13].
During orthodontic treatment, parastyle interfere with bonding of the brackets, molar banding and correct alignment of that particular tooth with other teeth in the arch. If the tooth with paramolar tubercle is banded with molar bands, the thickness of the paramolar tubercle will jeoparadise the alignment of the that particular tooth within the arch because of the tip, torque and in-out variations.
Following three procedures can be considered for the treatment of talon cusp if they are causing trauma, esthetic problems and trouble in bonding the orthodontic brackets [14].
Periodic reduction of accessory cusp over a 6-8-week interval with application of fluoride as a desensitizing agent, so that it will avoid possibility of pulpal exposure and helps in reparative dentine formation. Patient will be advised to use desensitizing tooth paste during this time period. Stepwise or gradual reduction of accessory cusp should be followed as it preserves the pulp vitality and averts the risk of pulp exposure and discomfort associated with deep dentinal preparation. The grinding of the cusp should be carried out along the side of the cusp and not the tip of the cusp so as not to damage the odontoblasts. The special care during reduction of cusp is taken because most of the odontoblasts lie along the length of the cusp. These odontoblasts promote deposition of reparative dentin over a period of few weeks [15].
1. Fissure sealants or glass-ionomer cement to seal associated grooves as prophylactic measure.
2. Complete reduction of cusp followed by calcium hydroxide pulpotomy for an immature tooth if pulpal exposure is encountered.
3. Once the cusp is flattened completely, it should be followed by root canal treatment to avoid non vitality of pulp in the future.
Conclusion
Parastyle, though very rare to be presented, needs proper diagnosis and treatment if the orthodontic treatment is planned to be carried out. The thickness of the paramolar tubercle will jeoparadise the alignment of the that particular tooth within the arch because of the tip, torque and in-out variations inbuilt in the preadjusted edgewise appliance of present generation.
- Nirmala SV, Gaddam KR, Vimaladevi P, Nuvvula S (2013) Protostylid: A case series. Contemp Clin Dent 4: 349‑352. Link: https://bit.ly/2VYogta
- Dahlberg A (1950) Analysis of the American Indian dentition. In: Brothwell DR, editor. Dental Anthropology. Oxford: Pergamon 149-177.
- Omal PM, Philipose L, Mathew AL, Nair S, Varghese AK, et al. (2013) Parastyle in a permanent maxillary first molar tooth: A rare entity. J Indian Acad Oral Med Radiol 25: 137-140.
- Gazala D, Hegde U, Mull P, Nabeel S (2014) Dental cusps: Normal, supernumerary and cusp-like structures – An overview. J Orofac Res 4: 161-168. Link: https://bit.ly/2VWpJjw
- Dahlberg AA (1945) The paramolar tubercle (bolk). Am J Phys Anthropol 3: 97‑103. Link: https://bit.ly/3jZL97I
- Kustaloghi OA (1962) Paramolar structures of the upper dentition. J Dent Res 41: 75–83. Link: https://bit.ly/3xVIt04
- Ash MM (1993) Wheeler's Dental Anatomy, Physiology and Occlusion. 7th ed. Philadelphia: WB Saunders. Link: https://bit.ly/3yTzTjq
- Bolk L (1914) Uberzahlige Zahne in der Molargegend des Menschen. Dtsch Monatsschr Zahnheilkd 32: 197.
- Turner CG, Regan M, Irish J (2011) Chapter nine: Physical Anthropology Analysis. Roosevelt Platform Mound Study: A Laboratory Plan for Salado Research. Archaeological Research Institute - Arizona State University. Internet resource. Link: https://bit.ly/2Xx8VjZ
- Mostowska A, Kobielak A, Trzeciak WH (2003) Molecular basis of non‑syndromic tooth agenesis: Mutations of MSX1 and PAX9 reflect their role in patterning human dentition. Eur J Oral Sci 111: 365‑370. Link: https://bit.ly/3mbOIKZ
- Jernvall J, Kettunen P, Karavanova I, Martin LB, Thesleff I (1994) Evidence for the role of the enamel knot as a control center in mammalian tooth cusp formation: Non-dividing cells express growth stimulating Fgf-4 gene. Int J Dev Biol 38: 463–469. Link: https://bit.ly/2Um37Zt
- Kerebel B, Dard M, Le Cabellec MT, Kerebel LM (1986) Dental enamel pearls: Histopathological study. J Biol Buccale 14 :239-248. Link: https://bit.ly/3m6LQ1S
- Rao PK, Mascarenhas R, Shetty SR (2011) Facial talon in mandibular incisor: An unusual occurrence. Dent Res J (Isfahan) 8: 229-231. Link: https://bit.ly/3m7mf96
- Shashikiran ND, Babaji P, Reddy VV (2005) Double facial and a lingual trace talon cusps: A case report. J Indian Soc Pedod Prev Dent 23: 89-91. Link: https://bit.ly/2UqkmZG
- Arora A, Sharma P, Lodha S (2016) Comprehensive and Conservative Management of Talon Cusp: A New Technique. Case Rep Dent 2016: 5843231. Link: https://bit.ly/3yQemZd
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
