Annals of Musculoskeletal Medicine
Incidence of Future Shoulder Procedures after SLAP Repair
Arjun Vohra*, Stephen Yao, Clayton Hui, Joshua Hustedt, Evan Lederman and Anup Shah
Department of Orthopedic Surgery, Sports Medicine, Banner University Medical Center, Orthopedic and Sports Medicine Institute, University of Arizona College of Medicine, Phoenix, AZ 85006, USA
Cite this as
Vohra A, Yao S, Hui C, Hustedt J, Lederman E, Shah A. Incidence of Future Shoulder Procedures after SLAP Repair. Ann Musculoskelet Med. 2025: 9(1): 012-016. DOI: 10.17352/amm.000036Copyright Licence
© 2025 Vohra A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Introduction: Previous literature has shown a high revision rate after a SLAP repair operation, which led to a decreased number of SLAP repairs being performed and an increased emphasis on patient selection. The transition to the ICD-10 coding system has allowed for more descriptive coding, enhancing the validity of the data mined from large databases. This study aims to assess the surgical revision rate, risk factors for revision, and subsequent procedures after a superior labrum anterior and posterior (SLAP) repair surgery.
Materials & methods: Data for the study were obtained from the national private insurance database Pearl Diver (years 2007 - 2020). All included patients underwent their first SLAP repair surgery with at least two years of follow-up. Patients were queried using Current Procedural Terminology (CPT) code 29807 and concurrent ICD-10 shoulder pathology diagnosis codes. The database was used to determine the revision rate of Subsequent Shoulder Procedures (SSP). The time between index surgery and subsequent procedures was noted. Finally, a logistic regression analysis with a significance cut-off of p ≤ 0.05 was conducted to determine the risk factors for a subsequent procedure after a SLAP repair.
Results: Out of 91 million patients, 15,958 patients (16,611 shoulders) met the criteria for the study. 1,389 (8.36%) repaired shoulders underwent a subsequent shoulder procedure on average 1.13 years after their initial SLAP repair. Younger age (OR = 1.01), elevated CCI (OR = 1.07), female gender (OR = 1.3), tobacco use (OR = 1.37), and obesity (OR = 1.21) significantly increased the risk of a subsequent shoulder procedure. Subacromial decompression, debridement, rotator cuff repair, manipulation under anesthesia, and revision SLAP repair were the most common subsequent procedures.
Discussion: An additional procedure may be necessary for approximately 1 in 12 patients a year after SLAP repair surgery. Patients who are younger, female, obese, have an increased CCI, and use tobacco are at increased risk of undergoing a revision procedure. Overall, the rate of revision procedures patients experience after a SLAP repair is less than initially reported.
Introduction
Superior labrum anterior to posterior (SLAP) tear repairs are a common procedure in the shoulder [1]. From 2002 to 2010, the popularity of these repairs grew immensely (with some studies suggesting SLAP repairs have an incidence of 1.2% -11.8% in arthroscopic shoulder surgery) [2]. However, after 2010 - 2012, the frequency of SLAP repair surgeries declined due to unfavorable outcomes and the need for secondary procedures [3]. As such, indications for SLAP repair surgery garnered much attention, and it has been reported that SLAP procedures make up < 3% of all shoulder procedures [4-8]. Several studies have reported a higher failure of the SLAP repair procedure, particularly in patients older than 35 to 40 [9-15]. Thus, SLAP repair has been indicated for athletes and younger patients, while biceps tenodesis (BT) is recommended for older patients [10,16].
Overall, research regarding outcomes and the need for revision surgery after a SLAP repair has produced mixed results, and factors associated with revision surgery require further investigation. Considering the advancements and increasing familiarity with arthroscopy techniques and technologies, it is important to re-evaluate the effects of the SLAP repair procedure in the modern setting. Recent transitions to the International Classification of Diseases 10th edition (ICD-10) coding system and software development have allowed for more accurate and versatile mining of large patient databases. This update has provided a unique opportunity to identify and analyze the side of the body affected by pathology (right/left) and procedural outcomes for SLAP repair surgeries.
This study aims to assess the surgical revision rate and subsequent procedures after a SLAP repair surgery. Given the increased awareness of SLAP repair indications and outcomes, improvements in arthroscopic technology and techniques, and improved patient selection, our team hypothesizes that the overall surgical re-operation is lower than previously thought.
Methods
The team data-mined an insurance-based patient record database aggregated by the Pearl Diver Database (www.pearldiverinc.com). The Pearl Diver Database compiles data from multiple insurance providers, including private and public sector information from sources such as Humana and Medicare. The version of the database used provided access to de-identified information from 91 million patients spanning 2007 to 2020. This database was chosen due to its ability to study diverse populations across the United States longitudinally. The data relevant to this study spans basic patient demographics, provider information, and procedural volumes. Information is sorted based on International Classification of Diseases, 9th Revision (ICD-9) diagnoses and procedures, International Classification of Diseases, 10th Revision (ICD-10) diagnoses and procedures, Current Procedural Terminology (CPT) codes, and National Drug Code directory (NDC). This study was exempt from institutional review board approval because it used de-identified data.
Study cohort
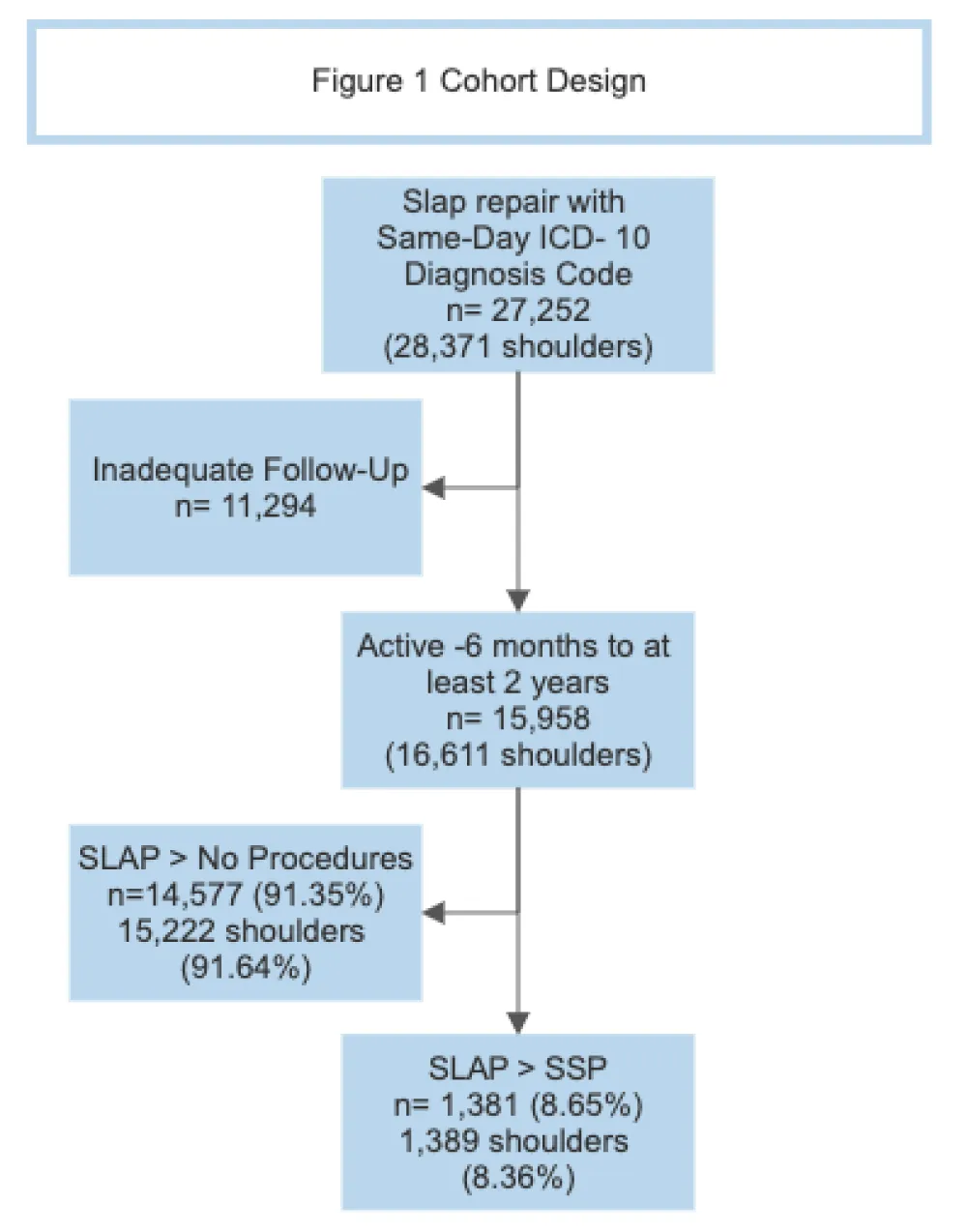
The base population was queried for patients who underwent their first arthroscopic SLAP repair procedure based on CPT-29807 with a concomitant same-day ICD-10 diagnosis code delineating if the shoulder pathology repaired occurred in the patient’s right or left shoulder (Appendix 1- Query). The ICD-10 coding system was used instead of the ICD-9 procedure because of the ability to distinguish which shoulder the surgery was performed on. Patients without this concomitant ICD-10 diagnosis code were excluded from the study. Patients were required to be active in the database for at least six months before the SLAP repair and at least two years after the procedure. This developed a base population of n = 15,958 patients (16,611 shoulders) (Figure 1). The demographics of this population are provided in Table 1.
Subsequent procedures after index surgery
The primary outcome of this study was the rate of subsequent shoulder procedures after a SLAP repair. This outcome was evaluated by examining all subsequent open, closed, and arthroscopic shoulder procedures (SSP) that the shoulder could have undergone after the index surgery. SSPs were defined by codes CPT-23000: CPT-23335, CPT-23395: CPT-23929, and CPT-29805: CPT-29828. This selection was determined to exclude injection-based procedures such as arthrocentesis/injections with and without ultrasound guidance (CPT- 20600-20611) and injection procedures for shoulder arthrography or enhanced CT/MRI shoulder arthrography (CPT-23350). All procedural codes were also run for same-day ICD-10 diagnosis codes to improve the likelihood that all subsequent procedures occurred in the same shoulder as the index SLAP repair (Figure 1). The demographics of these populations that underwent an SSP after SLAP repair are located in Table 1.
Statistical analysis
Pearl Diver has a built-in statistical software modeled after R. Our team decided to conduct a multivariable binomial generalized logistic regression analysis to identify risk factors for patients who experienced subsequent procedures after a SLAP repair. Variables included patient demographics such as age, Charlson Comorbidity Index (CCI), gender, diabetes, smoking, and obesity at or before the index procedure. Odds Ratios and 95% Wald CIs (based on asymptotic normality) were calculated for all prospective risk factors. A time between the index procedure and SSP was conducted.
Results
Demographics
Of the 91 million patients in the database, 15,958 patients (16,611 shoulders) underwent a SLAP repair and met the criteria for the study. This included 5,837 females and 10,121 males with an average age of 43. One thousand three hundred eighty-one patients (8.65%) (1,389 shoulders (8.36%)) underwent an SSP after their SLAP repair. These Patients were an average age of 42 at the time of their SLAP repair surgery. This included 583 females and 798 males. For a more detailed summary of cohort demographics (Table 1).
Statistical analysis
The average time between SLAP Repair and SSP was 414 days (1.13 years) (Table 2). Of the variables analyzed at the time of patient's SLAP repair, decreased age (p = 4.83 x 10-7, OR = 1.01), increased CCI (p = 0.0003 OR = 1.07), female gender (p = 5.63 x 10-6, OR = 1.30), tobacco use (p =1.68 x 10-7, OR = 1.37), and obesity (p = 0.002, OR = 1.21) significantly increased the risk of undergoing a SSP after a SLAP repair. A history of diabetes (p = 0.59) was not a significant risk factor for patients undergoing an SSP after their SLAP repair (Table 3).
SSP
The five most common SSP that patients underwent after their SLAP repair were arthroscopic decompression of subacromial space with partial acromioplasty with or without coracoacromial release (CPT - 29826) (n = 297), extensive arthroscopic debridement (CPT - 29823) (n = 266), arthroscopic rotator cuff repair (CPT - 29827) (n = 212), manipulation under anesthesia (MUA)(CPT - 23700) (n = 211), and arthroscopic repair of SLAP lesion (CPT - 29807)( n = 199). See Table 4.
Discussion
The current study demonstrates a decrease in revision rates of SLAP repair when compared to historical data. Heightened awareness regarding SLAP repair indications, outcomes, and advancements in technology, technique, implants, and patient selection over time may contribute to this decline. The current study validates this finding, demonstrating ~8% risk of patients undergoing an SSP less than 1.5 years after their index procedure, which is lower than historically reported outcomes of 37% failure rate and 28% re-operation rate for patients who underwent a SLAP repair, with an average time to failure time of 11.8 months in patients followed for an average of 3.5 years [14].
With rehabilitation and return to activity from the initial SLAP repair often approaching more than six months, further surgery has significant emotional, financial, and clinical implications. Assuming a 6-month recovery period after their second procedure, a patient who undergoes a second shoulder procedure 1.25 - 1.5 years after their initial surgery can spend ~2 years of their life resolving their initial pathology. While SLAP repairs confer a 2.08 QALY increase over continued non-operative treatment of SLAP tears, two years of shoulder disability is not inconsequential [12]. Shoulder lesions have been shown to significantly affect an individual’s mental and physical quality of life [17]. Additionally, one must also consider that the entire healthcare ecosystem feels the financial burden of healthcare resources from 2 years of office visits, imaging acquisition, physical therapy appointments, operating room costs, etc.
Younger patients, have increased CCI, are female, obese, and tobacco users at the time of their first SLAP procedure, were found to be at a significantly increased risk of undergoing a SSP. These risk factors, identified by our study, align with previous literature on this topic. While the analysis found that younger patients were at a statistically significant increased risk for undergoing an SSP with an OR of 1.01, with an OR so close to 1, the authors cannot provide recommendations on the clinical significance of this finding. Given the known historical failure rate or complication rate of SLAP repairs in patients over 40 years old, with multiple studies demonstrating satisfactory outcomes for biceps tenodesis in this group, an emphasis on biceps tenodesis for those patients has been recommended [10,12,14,18]. This could have resulted in a selection bias against older patients undergoing a SLAP repair, which may have affected the findings of our study, as our data incorporates data from 2015 onward.
With the focus historically highlighting biceps tenodesis after a failed SLAP repair, this is the first known study evaluating the risk of a comprehensive list of additional procedures on the shoulder post-SLAP repair, showing that biceps tenodesis was not among the top 5 procedures after a SLAP repair within 2 years of the index surgery. In our findings, three of the five most common procedures after a SLAP repair fall under the umbrella of commonly mentioned revision/follow-up procedures after a SLAP repair: subacromial decompression, extensive debridement, and revision SLAP repair. Two important findings were the presence of manipulation under anesthesia and rotator cuff repair, which are two of the most common procedures. While it is reasonable to ascertain that patients with shoulder pathology may develop post-operative stiffness requiring manipulation under anesthesia, it is important that future studies further evaluate concomitant pathology, iatrogenic injury, and post-operative protocols to address other pain generators, surgically related pathology, and reduce shoulder stiffness, respectively. These findings also suggest that further exploration may be needed to establish why a rotator cuff repair was indicated, because the findings may highlight the possibility of iatrogenic damage to the rotator cuff due to port placement as a possible complication of arthroscopic procedures, missed injury on initial evaluation, or another cause altogether. Because these top 5 procedures only comprise a proportion of all the SSPs performed, some may be related to misdiagnosed initial pathology, where the SLAP repair failed to address the patient’s surgical concern. Should this be the case, then the rate of SSP after SLAP repair in appropriately selected individuals may be less than what we have found in this study. This would support the fact that the field’s advancement is even further than estimated by this study.
Limitations
There are some limitations to the present study. As a retrospective review, selection bias for patients is an inherent issue that cannot be overlooked. Additionally, this database is based on insurance billing data, which is potentially not as accurate as other databases that have specialized intake personnel, such as the National Surgical Quality Improvement Program (NSQIP) database. It also lacks specific patient data, with the possibility of misdiagnosis and inconsistent indications for SLAP repair. Requiring a concomitant ICD-10 diagnosis code for both the initial and revision procedures to ensure that both the index and revision procedures occurred in the same arm eliminated all patients who may have had an unspecified diagnosis code at either time point. This limited our patient population and may have underestimated the overall revision rate. Lastly, the ICD-10 coding scheme has only been in effect since quarter 4 of 2015, and the database only has data until 2020, which limits the length of follow-up possible.
Conclusion
Despite these limitations, to the author’s knowledge, this is the largest and most comprehensive database study used to shed light on clinical outcomes nationally after SLAP repair. With a stronger focus on value and evidence-based medicine today, the current study advocates for stronger indications when considering SLAP repair in patients. Even with current advancements, 1 in 12 patients treated operatively for a SLAP repair undergo a SSP within 1.5 years from surgery. Patients should be counseled that the risk of subsequent surgery entails not only a biceps tenodesis but also other procedures. Additionally, surgeons must be aware of preoperative, intraoperative, and postoperative considerations that may lead to additional surgery in SLAP patients.
- Snyder SJ, Banas MP, Karzel RP. An Analysis of 140 Injuries to the Superior Glenoid Labrum. Journal of shoulder and elbow surgery. 1995;4(4):243-8. Available from: https://doi.org/10.1016/s1058-2746(05)80015-1
- Ablove RH, Aul A, Baer G. The Incidence and Demographics of Shoulder Repair in Wisconsin, 2002-2010. WMJ. 2014;113(6):223-226. Available from: https://pubmed.ncbi.nlm.nih.gov/25745695/
- Dougherty MC, Kulenkamp JE, Boyajian H, Koh JL, Lee MJ, Shi LL. National trends in the diagnosis and repair of SLAP lesions in the United States. Journal of Orthopaedic Surgery. 2020;28(1). Available from: https://doi.org/10.1177/2309499019888552
- Brockmeier SF, Voos JE, Williams RJ, Altchek DW, Cordasco FA, Allen AA. Outcomes after arthroscopic repair of type-II SLAP lesions. Journal of Bone and Joint Surgery - Series A. 2009;91(7):1595-1603. Available from: https://doi.org/10.2106/jbjs.h.00205
- Hong Lim M, Kuen Chan B, Edin F, Ooi Low C. Arthroscopic management of superior labral anterior and posterior (SLAP) and associated lesions: clinical features and functional outcome. Annals of the Academy of Medicine, Singapore. 2008;37(1):44-8. Available from: https://pubmed.ncbi.nlm.nih.gov/18265897/
- Neri BR, Vollmer EA, Kvitne RS. Isolated type II superior labral anterior posterior lesions: Age-related outcome of arthroscopic fixation. American Journal of Sports Medicine. 2009;37(5):937-942. Available from: https://doi.org/10.1177/0363546508328417
- Yong GR, Dong HL, Chan TL. Unstable isolated SLAP lesion: Clinical presentation and outcome of arthroscopic fixation. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2005;21(9):1099.e1-1099.e7. Available from: https://doi.org/10.1016/j.arthro.2005.05.016
- Yung PSH, Fong DTP, Kong MF, Lo CK, Fung KY, Ho EPY, et al. Arthroscopic repair of isolated type II superior labrum anterior-posterior lesion. Knee Surgery, Sports Traumatology, Arthroscopy. 2008;16(12):1151-1157. Available from: https://doi.org/10.1007/s00167-008-0629-4
- Cohen DB, Coleman S, Drakos MC, Allen AA, O'Brien S, Altchek DW, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2006;22(2):136-142. Available from: https://doi.org/10.1016/j.arthro.2005.11.002
- Erickson J, Lavery K, Monica J, Gatt C, Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: A systematic review. American Journal of Sports Medicine. 2015;43(5):1274-1282. Available from: https://doi.org/10.1177/0363546514536874
- Kim SH, Ha KI, Kim SH, Choi HJ. Results of Arthroscopic Treatment of Superior Labral Lesions. The Journal of bone and joint surgery. American volume. 2002;84(6):981-5. Available from: https://doi.org/10.2106/00004623-200206000-00012
- Paoli AR, Gold HT, Mahure SA, Mai DH, Agten CA, Rokito AS, et al. Treatment for Symptomatic SLAP Tears in Middle-Aged Patients Comparing Repair, Biceps Tenodesis, and Nonoperative Approaches: A Cost-Effectiveness Analysis. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2018;34(7):2019-2029. Available from: https://doi.org/10.1016/j.arthro.2018.01.029
- Park JY, Chung SW, Jeon SH, Lee JG, Oh KS. Clinical and radiological outcomes of type 2 superior labral anterior posterior repairs in elite overhead athletes. American Journal of Sports Medicine. 2013;41(6):1372-1379. Available from: https://doi.org/10.1177/0363546513485361
- Provencher MT, McCormick F, Dewing C, McIntire S, Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: Outcomes and factors associated with success and failure. American Journal of Sports Medicine. 2013;41(4):880-886. Available from: https://doi.org/10.1177/0363546513477363
- Taylor SA, Degen RM, White AE, McCarthy MM, Gulotta LV, O'Brien SJ, et al. Risk Factors for Revision Surgery after Superior Labral Anterior-Posterior Repair: A National Perspective. American Journal of Sports Medicine. 2017;45(7):1640-1644. Available from: https://doi.org/10.1177/0363546517691950
- McCormick F, Nwachukwu BU, Solomon D, Dewing C, Golijanin P, Gross D, et al. The efficacy of biceps tenodesis in the treatment of failed superior labral anterior posterior repairs. American Journal of Sports Medicine. 2014;42(4):820-825. Available from: https://doi.org/10.1177/0363546513520122
- Rincón-Hurtado ÁM, Rocha-Buelvas A, López-Cardona A, Martínez JW. Health-related quality of life of patients with rotator cuff injuries, Cofee Triangle, Colombia, 2013. Revista Brasileira de Ortopedia. 2018;53(3):364. Available from: https://doi.org/10.1016/j.rboe.2018.03.018
- Brockmeyer M, Tompkins M, Kohn DM, Lorbach O. SLAP lesions: a treatment algorithm. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(2):447-455. Available from: https://doi.org/10.1007/s00167-015-3966-0
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.

 Save to Mendeley
Save to Mendeley
