Annals of Musculoskeletal Medicine
Lateral Closing Wedge High Tibial Osteotomy and Non-customized Total Knee Arthroplasty in a Patient with Achondroplasia. Single-stage Surgical Planning
1Department of Orthopedic Surgery, Elda University Hospital, Ctra Elda-Sax s/n, 03600 Elda, Alicante,Spain
2Department of Orthopedic Surgery, Vithas Medimar Hospital, Avenida de Denia, 78. 03016 Alicante,Spain
3Department of Rehabilitation and Physiotherapy, Elda University Hospital, Ctra Elda-Sax s/n, 03600 Elda, Alicante, Spain
Author and article information
Cite this as
Miralles-Muñoz FA,Ferragut-Bria C,Zofío-Bellod JA. Lateral Closing Wedge High Tibial Osteotomy and Non-customized Total Knee Arthroplasty in a Patient with Achondroplasia. Single-stage Surgical Planning. Ann Musculoskelet Med. 2025; 9(2): 017-021. Available from: 10.17352/amm.000037
Copyright License
© 2025 Miralles-Muñoz FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Patients with achondroplasia often experience knee osteoarthritis, which is marked by varus deviation of the tibia, as well as recurvatum, internal tibial torsion, and mediolateral instability of the knee. This presents a challenge for surgeons, as it necessitates meticulous planning of intricate procedures that may need to be carried out in one or multiple surgical stages.
There are few descriptions in the literature of a single-stage complex knee treatment for patients with achondroplasia. Additionally, there is a lack of information on the method used for precisely calculating the dimensions of the bone wedge to be resected during the lateral tibial closure osteotomy procedure.
We present the case of a 52-year-old man with achondroplasia (height 122 cm) and deforming osteoarthritis of the knees. The right knee showed severe malalignment with a 36.4° extra-articular varus deformity and multidirectional instability. A single-stage surgery was necessary, involving meticulous planning for a tibial osteotomy and a total knee arthroplasty with a rotating hinge. The clinical and radiological outcomes at 2 years postoperative follow-up were satisfactory.
This study outlines the methodology used for single-stage surgical planning with a lateral closing wedge technique, followed by a non-customized total knee arthroplasty in a case of deforming osteoarthritis of the knee with very small anatomical dimensions in a young patient with achondroplasia.
Achondroplasia is the most common hereditary skeletal dysplasia. It is characterized by abnormal endochondral ossification, which leads to rhizomelic dwarfism with shortening of the proximal limb bones and a normal-sized trunk. At the lower limb level, 40% - 70% of patients present with varus deviation of the tibia, associated with recurvatum, internal tibial torsion, and mediolateral knee instability [1].
The decision to undergo surgery is determined by the severity of degenerative changes and deformity, as well as the current symptoms and functional limitations. Patients may present with severe misalignment with soft tissue laxity and/or contractures and low bone density [2]. Furthermore, smaller custom-made prosthetic components are often required.
This poses a challenge for the surgeon, especially when considering the size and placement of the implants, as well as the balance of the surrounding soft tissues. It may require complex surgeries involving a combination of procedures in one or more surgical stages. Therefore, the different surgical options must be planned independently, taking into account anthropometric, radiological, functional, and quality-of-life variables. Special considerations must be taken when performing total knee arthroplasty (TKA) in patients with this skeletal dysplasia.
There are few descriptions in the literature of a single-stage complex knee treatment for patients with achondroplasia. Additionally, there is a lack of information on the method used for precisely calculating the dimensions of the bone wedge to be resected during the lateral tibial closure osteotomy procedure.
This study outlines the methodology used in for surgical planning of single stage with lateral closing wedge technique, followed by a non-customized total knee arthroplasty in a patient with achondroplasia and knee deforming osteoarthritis.
Case report
A 52-year-old male with achondroplasia presented with severe pain and functional impairment caused by deforming osteoarthritis in both knees, particularly the right knee. Conservative treatment was deemed ineffective, so prehabilitation sessions were started in the rehabilitation service to enhance muscle tone and range of motion before surgical intervention.
During the physical examination, the patient’s height was measured at 1.22 meters, weight at 46 kilograms, and body mass index was calculated to be 22.1. The right knee showed severe malalignment with a 36.4° extra-articular varus deformity, multidirectional instability, and a range of motion from 0° to 80°. The left knee displayed clinical and radiological signs of moderate osteoarthritis, with minimal discomfort. There were no discrepancies in the length of the lower limbs. In addition, he had previously undergone bilateral total hip arthroplasty, with satisfactory clinical results.
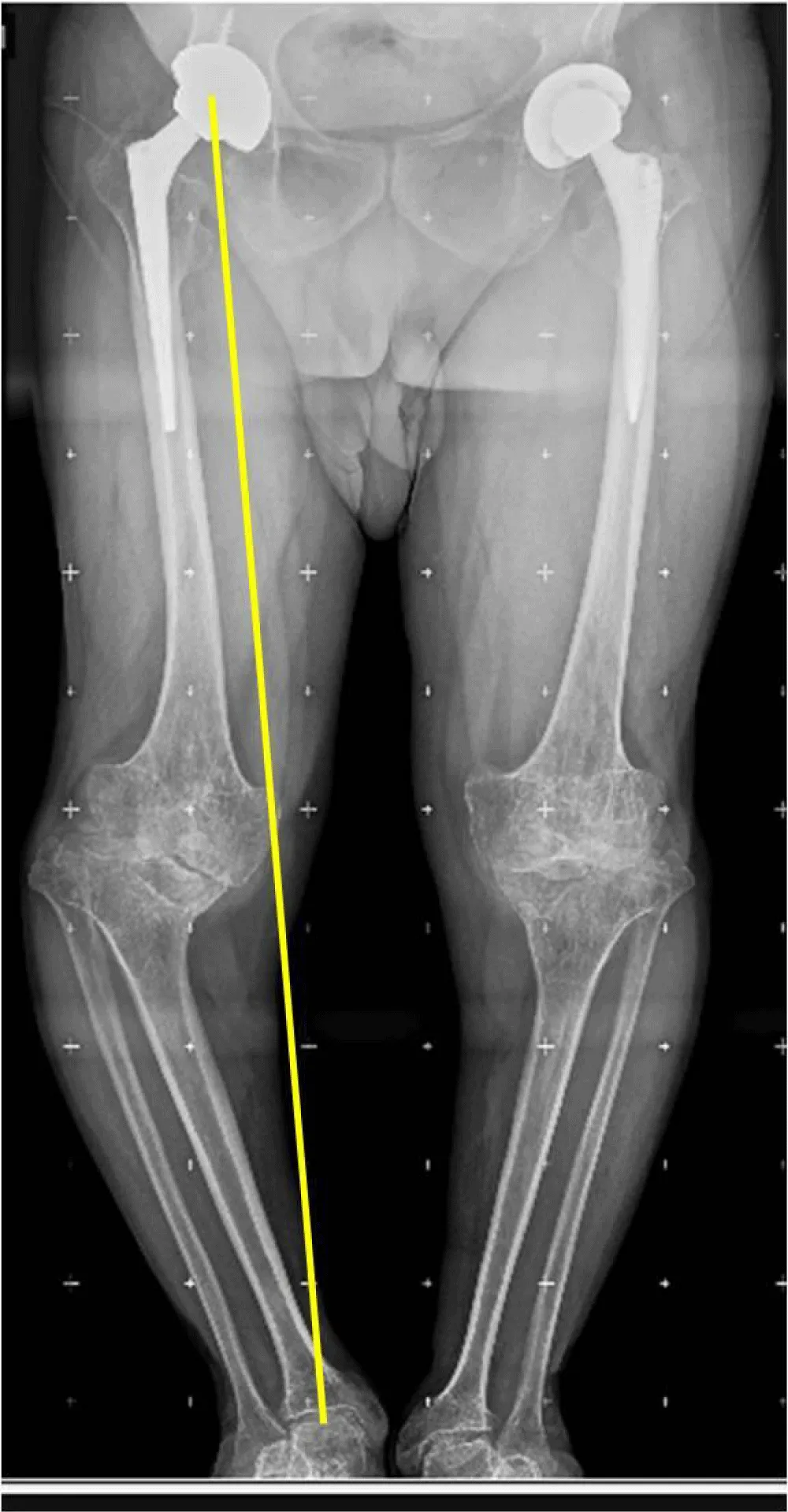
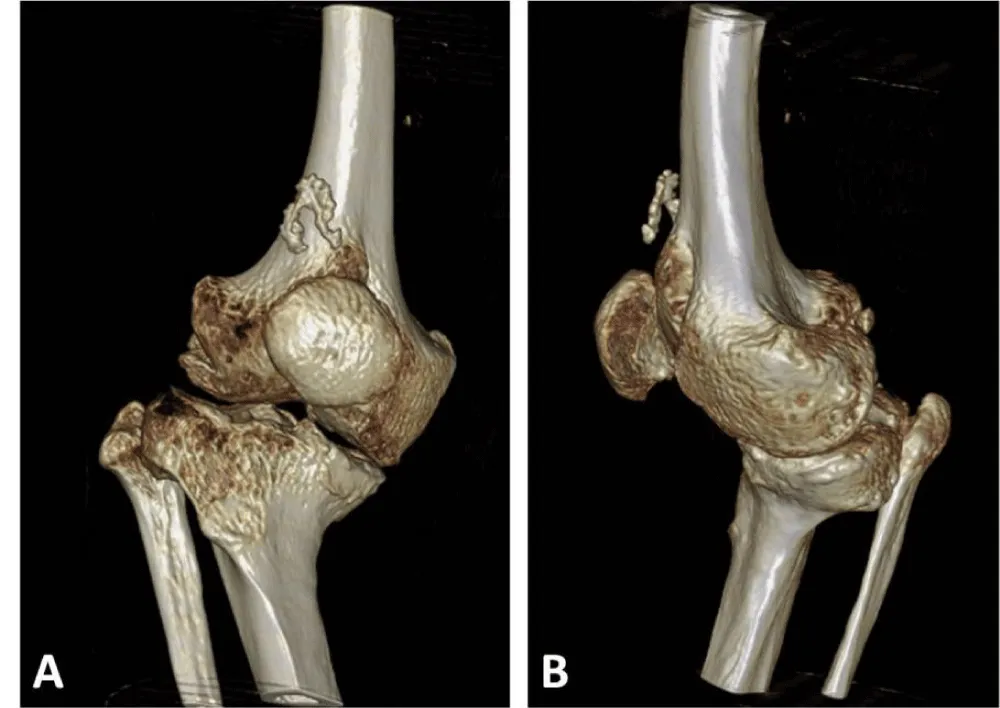
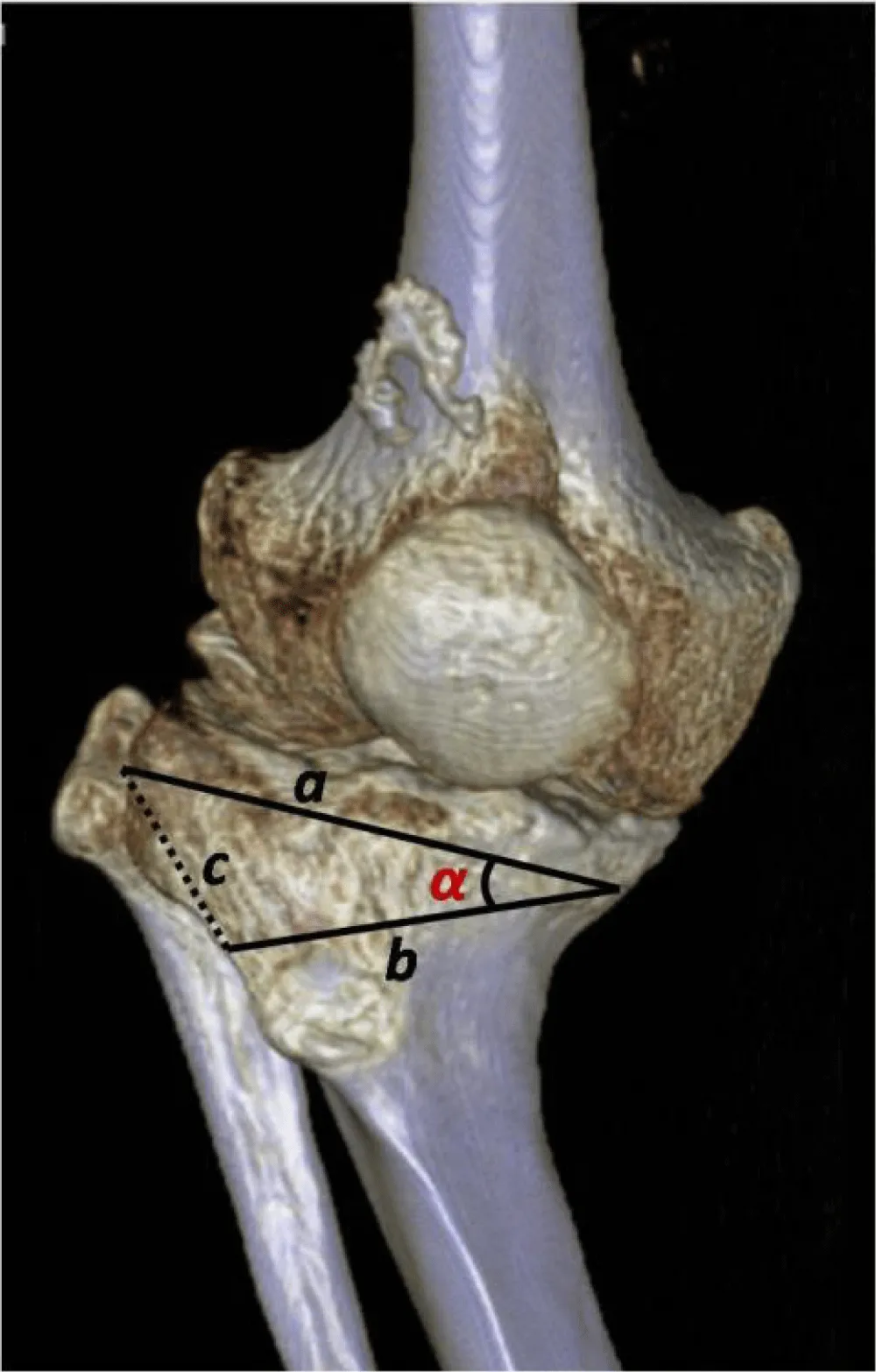
X-rays reveal severe deforming osteoarthritis of the right knee with a medial tibial metaphyseal angle of 53.6° (Figure 1). Telemetry shows medialization of the weight-bearing axis of the right lower extremity due to severe genu varum (Figure 2). Computed tomography (CT) confirms joint destruction with varus deformity of the proximal tibia (Figure 3), and severe misalignment of the posterior tibial slope (Figure 4).
Following a physical examination and analysis of imaging tests, it was determined that a double surgical procedure was necessary in a single operation: a lateral closing wedge high tibial osteotomy along with a non-customized rotating hinge type TKA.
Planning of the surgical procedure
The calculation of the dimensions of the tibial bone wedge to be resected was completed in two stages.
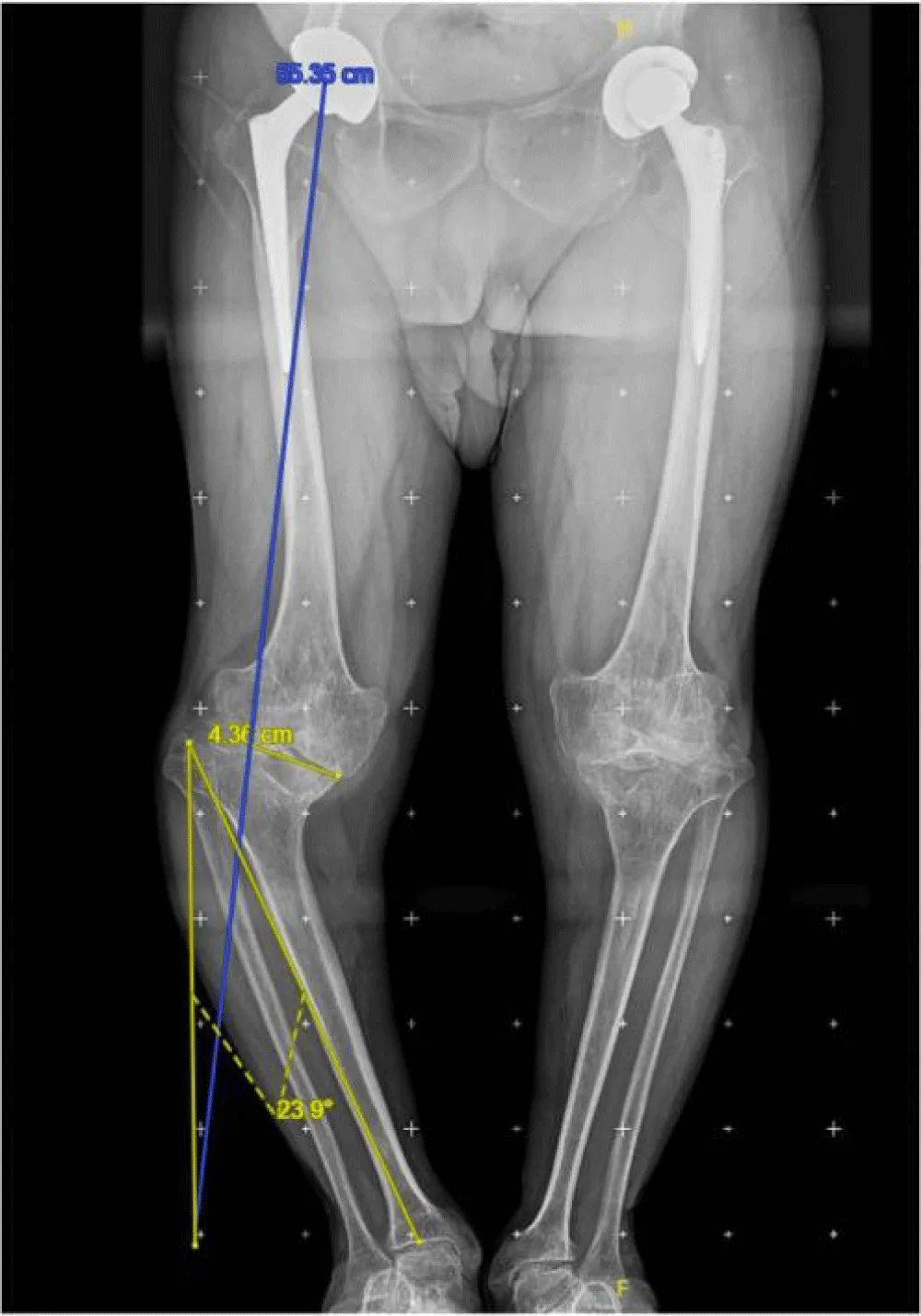
A) First step: Miniaci method (Figure 5).
Planning was performed using the Miniaci method on a weight-bearing radiograph of the entire lower extremity, as follows:
- Draw a line from the center of the femoral head to the center of the ankle joint.
- Establish the desired position of the mechanical axis by using the center of the femoral head and the Fujisawa point on the knee as references.
- Choose the osteotomy point on the lateral aspect of the tibia, typically above the fibular head.
- Connect the osteotomy point to the center of the ankle and the preoperative weight-bearing axis. The resulting angle between these two lines is the correction angle, which indicates the amount of bone wedge that needs to be resected in order to normalize the mechanical axis [3]. The calculations determined that a correction angle of 23.9° was required.
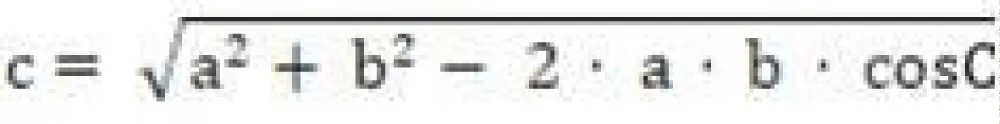
B) Second step: Trigonometric calculation.
Given the sides a and b (measured in the AP projection of the last preoperative X-ray) and the angle C between them (calculated using the Miniaci method), the cosine theorem (Figure 6) must be applied to calculate side c (Figure 7).
Calculations determined that the base of the tibial bone wedge to be resected should measure 3.1 cm. During an opening tibial osteotomy, specific instrumentation is utilized to achieve precise angular correction based on the Miniaci method. This eliminates the need for extra calculations that are necessary for a closing osteotomy.
Surgical procedure
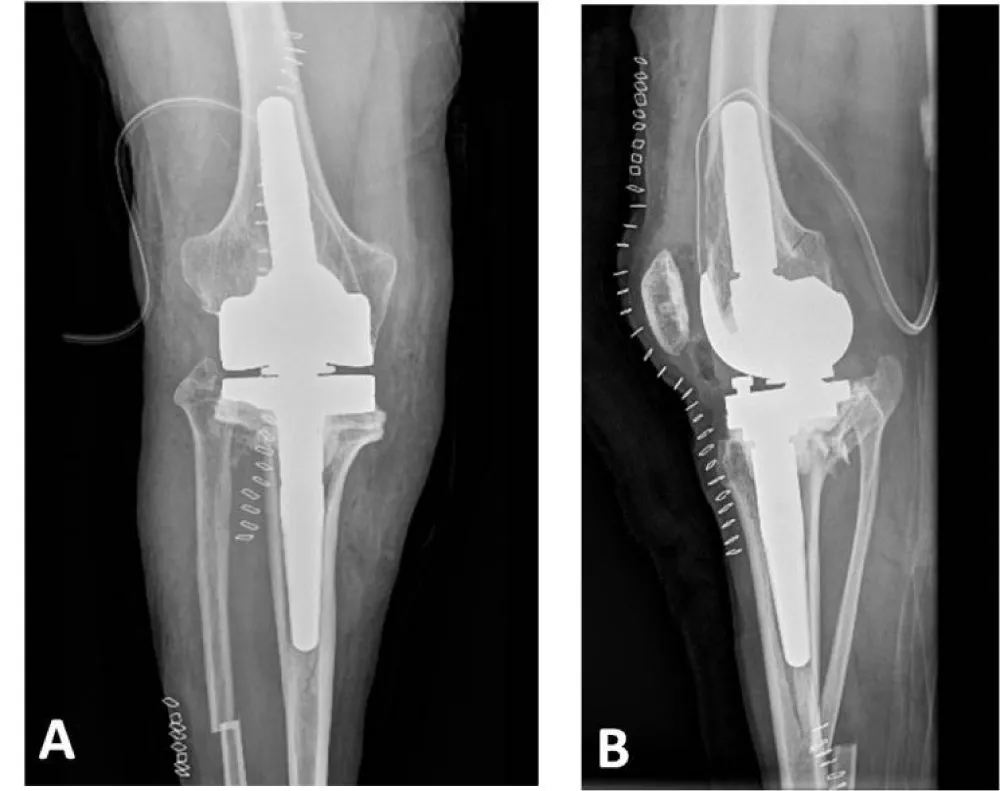
The surgery was performed on the right knee under spinal anesthesia, with the patient in the supine position and an ischemia cuff applied to the thigh. Initially, the lateral closing wedge high tibial osteotomy was completed. After normalizing the axes, a rotating hinge total knee prosthesis (Rotating Hinge Knee, Waldemar Link, Hamburg, Germany) was implanted.
The lateral closing wedge high tibial osteotomy was performed in a standardized manner after the subtraction osteotomy on the fibular shaft. According to the calculations explained above, a 3.1 cm laterally based bone wedge was resected without the use of a fixation system. This type of closing osteotomy was chosen over opening osteotomy because it made it easier to implant the tibial component and did not cause length discrepancies in the lower limbs after correcting the tibial varus.
Subsequently, an X-small-sized rotating hinge total knee arthroplasty was implanted. Despite the small bone size, the femoral cage was successfully completed without fracturing or weakening the femoral condyles. Uncemented stems, measuring 14 mm thick and 50 mm long in the femur, and 10 mm thick and 80 mm long in the tibia, were placed. Additionally, a 20 mm distal lateral femoral augment and a 5 mm medial tibia augment were necessary. Bone sections were completed using intramedullary guides (Figure 8).
After surgery, the knee’s functional recovery began with physical therapy sessions. The postoperative X-ray revealed a fissure line distal to the tibial stem, so weight-bearing was prescribed for 4 weeks, with full weight-bearing permitted starting in the 5th postoperative week.
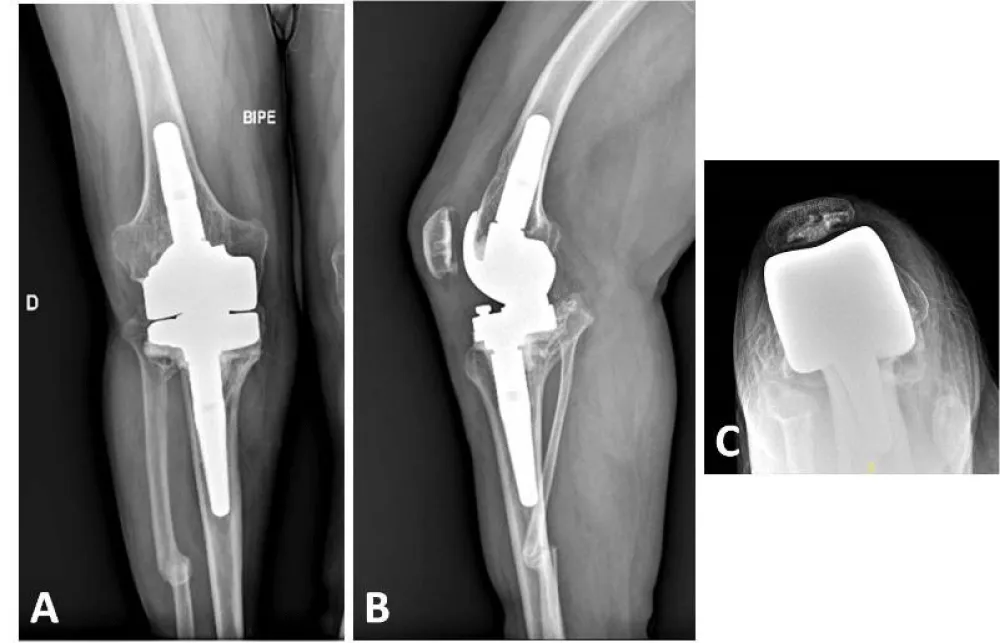
Twelve months postoperatively, the patient was able to walk without pain or the need for external assistance. The patient’s range of motion was acceptable, with active extension of 0° and flexion of 90°. The radiological evaluation revealed the absence of radiolucent lines or migrations of prosthetic components, along with consolidation of the fracture line distal to the femoral stem (Figure 9). With two years of follow-up, the patient is leading an active life without significant limitations due to his knee surgery, and is highly satisfied with the clinical outcome.
Discussion
Achondroplasia is a rare bone dysplasia that often presents with associated misalignments, low bone density, and can progress to early osteoarthritis. These factors can complicate the surgical procedure, posing a significant challenge for the orthopedic surgeon and requiring complex surgeries with smaller prosthetic components. Therefore, careful preoperative planning and meticulous technical considerations are essential.
There are several surgical options for addressing knee deformities in patients with achondroplasia, including TKA without correcting mild deformities or correcting significant misalignments in one or two stages. Varus alignment of the knee can be caused by tibial deformities, combined tibiofemoral deformities, or ligament imbalances. Understanding the malalignment is essential in TKA to restore the neutral mechanical axis in the frontal plane. The most common knee morphotype in achondroplasia patients is genu varum with widened metaphyses. Occasionally, extra-articular metaphyseal varus angulation may be linked to lateral collateral ligament insufficiency and flexion contractures, which can restrict range of motion. Therefore, technical challenges in TKA for these patients include soft tissue contractures, ligament laxity, extra-articular deformities, and difficulties with standard prosthesis sizing due to bone size and joint structural abnormalities. It is widely agreed that CT scans are crucial for preoperative planning in these cases, helping assess bone mass, deformities, and implant sizes to ensure proper prosthetic component fit in the femur and tibia medullary canals. Custom implants are often necessary in cases of skeletal dysplasia.
In the comparative study by Tan, et al. [2], no statistically significant differences in revision rates were observed in achondroplastic patients. However, a higher likelihood of stiffness due to component oversizing was noted, suggesting the use of smaller or custom-made implants to accommodate morphological differences in this patient population. The authors recommend several measures to prevent oversizing, such as preoperative CT scans, hand-cutting of femoral bones, and custom-designed implants. On the other hand, Guenther, et al. [4], in their study of 138 knee replacements in patients 150 cm or shorter, found a lower survival rate compared to the general population. Despite this, they argue that knee replacement can still be successfully performed in patients with dwarfism, yielding good clinical results. In a study by Ali, et al. [5], excellent implant survival and satisfactory clinical outcomes were reported after total knee arthroplasty, with a follow-up exceeding 20 years. This was achieved despite the technical challenges and associated complexity of the procedure.
Some authors, such as Wallace, et al. [6], argue that a staged correction of extra-articular deformity is a safer and more effective approach to improving limb alignment before knee replacement surgery. Zmerly, et al. [7], on the other hand, believe that the one-stage procedure increases the risk of complications such as joint stiffness, deep vein thrombosis, malunion, and surgical site infection. Similarly, Lausman, et al. [8] reported higher rates of implant-associated complications and revision surgeries compared to the general population.
Single-stage TKA is a technically more complex treatment for patients with knee osteoarthritis and mild extra-articular deformity. Xiao, et al. [9] recommend TKA with intra-articular bone resection and adequate soft tissue balance. They argue that a simultaneous corrective osteotomy with TKA is necessary for the treatment of severe extra-articular deformity associated with knee osteoarthritis, achieving an adequate physiological mechanical axis without causing substantial bone loss [9].
In cases of significant misalignment, it is recommended to consider more constrained implants due to the need for soft tissue releases to address the complex imbalance of the collateral ligaments. In such situations, a rotating hinge TKA can be a suitable treatment option [5,10]. Ali, et al. [5] conducted a study on 31 knees in 22 patients with bone dysplasia who underwent TKA, including 8 with achondroplasia. Out of the 31 cases, 17 procedures involved a hinge-type prosthesis, 9 received posterior-stabilized TKA, and 5 underwent cruciate ligament-retaining TKA, all with cemented fixation. Thirteen knees needed custom implants as the standard prosthetic components were too large relative to the medullary canal diameter and articular surface size. None of the cases required an additional procedure for deformity correction. Some authors recommend using of a navigation device in patients with severe and irreducible bone deformities, to perform a precise tibial osteotomy in combination with a primary TKA [11], improving precision with less intraoperative radiation [12].
Unlike hip replacement surgery, evidence on the outcomes of TKA in patients with bone dysplasia is more limited. It has not been firmly established whether the results are comparable to those of patients of normal height, and whether short stature may indicate lower prosthesis survival and higher complication rates. Ali, et al. [5] found inferior functional outcomes after TKA in patients with bone dysplasia compared to the general population with a mean follow-up of 9 years. However, the authors concluded that these results did not contraindicate this treatment in patients with achondroplasia.
Conclusion
This study outlines the methodology used in for surgical planning of single stage with lateral closing wedge technique, followed by a non-customized total knee arthroplasty in a patient diagnosed with achondroplasia and knee deforming osteoarthritis. At the 2-year postoperative follow-up, satisfactory clinical and radiological results were observed, with a high level of patient satisfaction.
We believe the significance of this study lies in the method used to calculate the bone wedge that needs to be resected in order to restore the knee axes during a single-stage procedure for a patient with achondroplasia and severe, deforming osteoarthritis of the knee.
Ethical statement
This research has been approved by the authors’ affiliated institutions and informed consent was required for participation in the study. This study adhered to the guidelines of the Declaration of Helsinki.
Author’s contributions
All authors have contributed to the conception and design of the study, data acquisition, data analysis and interpretation, writing and critical review of the article, and final approval of the submitted version.
- Savarirayan R, Ireland P, Irving M, Thompson D, Alves I, Baratela WAR, et al. International consensus statement on the diagnosis, multidisciplinary management and lifelong care of individuals with achondroplasia. Nat Rev Endocrinol. 2022;18(3):173–189. Available from: https://doi.org/10.1038/s41574-021-00595-x
- Tan TL, Kheir MM, Modi R, Chen CL, Shao H, Chen AF. Midterm survivorship and complications of total knee arthroplasty in patients with dwarfism. J Arthroplasty. 2017;32(11):3364–3367. Available from: https://doi.org/10.1016/j.arth.2017.06.002
- Elson DW, Petheram TG, Dawson MJ. High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci's method. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):2041–2048. Available from: https://doi.org/10.1007/s00167-014-2920-x
- Guenther D, Kendoff D, Omar M, Cui LR, Gehrke T, Haasper C. Total hip arthroplasty in patients with skeletal dysplasia. J Arthroplasty. 2015;30(9):1574–1576. Available from: https://doi.org/10.1016/j.arth.2015.03.024
- Ali E, Adedoyin G, Sivayoganathan S, Mudiganty S, Jayadev C, McCulloch RA. Total knee arthroplasty in patients who have skeletal dysplasia: a center's experience with a mean 9-year follow-up. J Arthroplasty. 2024;39(11):2745–2754. Available from: https://doi.org/10.1016/j.arth.2024.05.051
- Wallace SJ, Greenstein MD, Fragomen AT, Reif TJ, Rozbruch SR. Staged extra-articular deformity correction in the setting of total knee arthroplasty. Arthroplast Today. 2023;24:101247. Available from: https://doi.org/10.1016/j.artd.2023.101247
- Zmerly H, Russo M, Moscato M, Akkawi I. Total knee arthroplasty in a young patient with achondroplasia. BMJ Case Rep. 2021;14(7):e242909. Available from: https://doi.org/10.1136/bcr-2021-242909
- Lausmann C, Niculescu S, Citak M, Rossmann M, Gehrke T, Zahar A. Revision arthroplasty with total femur replacement for the management of complex post-traumatic bone defect in a patient with dwarfism. Z Orthop Unfall. 2021;159(5):533–536. Available from: https://doi.org/10.1055/a-1154-8994
- Xiao-Gang Z, Shahzad K, Li C. One-stage total knee arthroplasty for patients with osteoarthritis of the knee and extra-articular deformity. Int Orthop. 2012;36(12):2457–2463. Available from: https://doi.org/10.1007/s00264-012-1695-2
- Nuutinen TK, Madanat R, Både KW, Ristolainen LH, Kauppinen H, Manninen MJ. Custom-made hinged total knee arthroplasties in the context of extra-articular deformity: a case series. Eur J Orthop Surg Traumatol. 2023;33(4):1411–1420. Available from: https://doi.org/10.1007/s00590-022-03299-8
- Denjean S, Chatain F, Tayot O. One-stage computer-assisted total knee arthroplasty and tibial osteotomy. Orthop Traumatol Surg Res. 2017;103(3):381–386. Available from: https://doi.org/10.1016/j.otsr.2017.01.007
- Hernigou J, Morel X, Hernigou P. Computer navigation technique for simultaneous total knee arthroplasty and opening wedge high tibial osteotomy in patients with large tibial varus deformity. Surg Technol Int. 2020;37:265–274. Available from: https://pubmed.ncbi.nlm.nih.gov/33238026/
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
