Archives of Otolaryngology and Rhinology
Ganglioneuroma of the neck: A case report
Ilknur Haberal Can1*, Yunus Kantekin2, Betul Aytekin3, Serdar Yanik4 and Kivanc Atilgan5
2Attending physician, Bozok University Medical Faculty Otolaryngology Head Neck Surgery, Yozgat, Turkey
3Resident, Bozok University Medical Faculty, Department of Pathology, Yozgat, Turkey
4Attending physician, Bozok University Medical Faculty, Department of Pathology, Yozgat, Turkey
5Attending physician, Bozok University Medical Faculty, Department of Cardiovascular Surgery, Yozgat, Turkey
Cite this as
Can IH, Kantekin Y, Aytekin B, Yanik S, Atilgan K (2019) Ganglioneuroma of the neck: A case report. Arch Otolaryngol Rhinol 5(2): 059-061. DOI: 10.17352/2455-1759.000098Objectives: An unusual left parapharyngeal ganglioneuroma case was discussed in the context of diagnostic difficulties, surgical tricks and Horner syndrome as a main surgical complication.
Methods: The patient presented with a painless neck mass. Fine needle aspiration did not give any clue regarding diagnosis. The mass was removed totally by a challenging surgery.
Results: Histopathology revealed ganglioneuroma. Horner syndrome occurred after surgery.
Conclusion: Due to the scarcity of ganglioneuromas and the lack of specific signs and symptoms, it is often difficult to reach a definitive diagnosis prior to pathological examination. Ganglioneuromas should be considered in differential diagnosis of cervical neck masses located medial to main neurovascular structures. The patients should be warned of the possible complication of Horner syndrome.
Introduction
Ganglioneuromas (GNs) originate from primordial neural crest cells, which migrate from the mantle layer of the developing spinal cord to the symphatic ganglia, adrenal medulla and other sites [1]. They are benign tumors, having only mature neural elements. It has rarely been associated with neurofibromatosis type 1, an autosomal dominant inherited disease. GNs have been reported in mediastinum, abdomen, but rarely in the neck [2].
In this case report, an unusual left parapharyngeal ganglioneuroma was discussed in the context of diagnostic difficulties, surgical tricks and Horner syndrome.
Case Report
A 32-year-old female patient was admitted to the ENT clinic with a complaint of mass in her left neck. The mass was gradually growing for the last few months. ENT and cranial nerve examinations were normal except the painless upper neck mass. MRI revealed a mass in the left parapharyngeal and upper cervical region (Figure 1). Also, there were 2 other masses in the T1 cervical foraminas. There were no any further details of its feature. Fine needle aspiration biopsy was reported as reactive lymph node. At the time of operation, the mass was located medial to external and internal carotid arteries, common carotid artery, jugular vein and vagal nerve (Figure 2). The arteries and jugular vein were pushed outward and extremely reduced in their diameters. There were 2 lymph nodes close to the mass.
At first glance, it seemed that the mass originated from medial part of the carotid body. However it was easily separated from the carotid arteries with blunt dissection. Dissection was challenging in the medial part of the mass and at the skull base due to the narrow working space. The mass was totally removed by cervical approach. 9., 10., 11. and 12. cranial nerves and branchial plexus were preserved. Mostly blunt dissection was performed during surgery. In the first postoperative day, the patient developed pitosis, which is a component of Horner syndrome. However there were no anhidrosis and myosis.
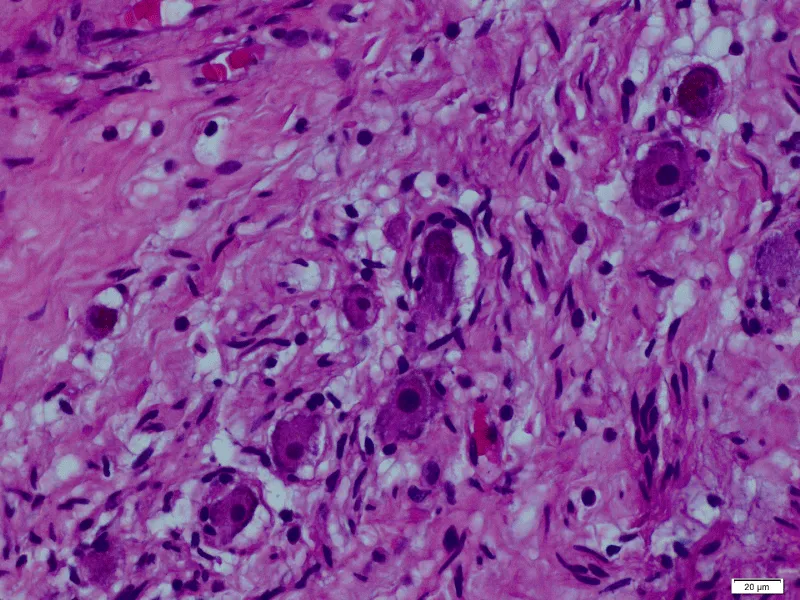
Macroscopic examination showed a hard, oblong, 6x4x3 cm well circumscribed mass surrounded by a pseudo capsule. Histopathologic investigation was reported as ganglioneuroma (Figure 3). Ganglion cells were identified within scattered neurofibrous stroma. After 6 months of follow up, Horner syndrome persisted. Follow up was recommended for the masses in cervical foraminas by neurosurgery department.
Discussion
GNs are most commonly located in posterior mediastinum followed by retroperitoneum. GN of the parapharyngeal space commonly originates from sympathetic trunk. When a tumor is functioning, a patient with a palpable neck mass may also have diarrhea, sweating, hypertension, flushing and renal acidosis (3). Our case did not show secretory function related symptoms.
In the literature, GN of head and neck usually presents with slowly growing painless mass. When a mass compresses surrounding tissues, especially to vascular and cranial nerves, unique symptoms related to these structures may occur. Symptoms of Horner syndrome may also occur related either to preoperative sympathetic trunk compression of the mass or to surgery [4]. Horner syndrome is characterized by ptosis, myosis, ipsilateral facial anhydrosis and flushing [5].
Due to the scarcity of GN cases and the lack of its specific signs and symptoms, it is often difficult to reach a definitive diagnosis without pathological examination. CT and MRI enable valuable information on the size, location, composition of the mass and its relation to adjacent significant vascular and neural structures. The need for an experienced radiologist is vital for defining the extent of the mass correctly and at the same time for guiding the ENT surgeon during such a challenging surgery. GN should be suspected when a mass is observed in low intensity on T1 weighted images, marked high intensity on T2 weighted images and gradual enhancement on diffusion MRI [4]. Rare case reports are invaluable guides to interpret the radiologic data better to lead to preoperative accurate differential diagnosis of head and neck masses.
The most characteristic histological features of GNs are mature ganglion cells. They are macroscopically encapsulated. Differential diagnosis usually includes branchial cysts, carotid body tumor, cystic higroma, tubercular adenitis, pharyngeal diverticulum and lymphoma [2]. Although fine needle aspiration biopsies are generally useful, cost effective and rapid procedures, they often give misleading results for GNs [6]. Therefore, fine needle aspiration biopsy as a diagnostic procedure is not always conclusive.
Surgical excision of GN is the first choice of its treatment [7]. Adjuvant chemo or radiation therapy is not even needed. Depending on the tumor location transcervical, transoral, tranparotid, transcervical-transpharyngeal and infratemporal fossa approaches may be used [8]. The risks for any complications are mainly due to either intraoperative injury or sacrificing neural and vascular structures associated with the tumor. Since the tumor´s origin is from the sympathetic chain, surgical excision may result in Horner’s syndrome. Therefore, it is important to counsel patients regarding the risk of Horner syndrome prior to surgery.
Conclusion
GNs should be considered in differential diagnosis of cervical neck masses located medial to main neurovascular structures such as carotid arteries, vagus and jugular vein. The patients should be warned of the possibility of vascular and neurogenic postoperative complications especially for Horner syndrome.
- Gary C, Robertson Ruiz B, Suzuki V, Walvekar RR (2010) Retropharyngeal ganglioneuroma presenting with neck stiffness: report of a case and review of the literature. Skull base 20: 371-374. Link: https://bit.ly/2IRRhNS
- Sinha P, Sharma S, Agarwal S, Gupta SD (2011) Parapharyngeal ganglioneuroma with neurofibromatosis: an unusual presentation. Ann Otol Rhino Laryngeal 120: 769-774. Link: https://bit.ly/2FCCnZW
- Kaufman MR, Rhee J, Fliegelman RJ, Constantino PD (2001) Ganglioneuroma of the parapharyngeal space in a pediatric patients. Otolaryngology Head and Neck Surgery 124: 702-704. Link: https://bit.ly/2J8DTnx
- Ma J, Liang L, Liu H (2012) Multiple cervical ganglioneuroma: a case report and review of the literature. Oncology letters 4: 509-512. Link: https://bit.ly/2ITaO0H
- Katilmis H, Ozturkcan S, Adadan I, Ozdemir I, Algin H, et al. (2006) Cervical ganglioneuroma. Int J Ped Otorhinolaryngol extra 1: 157-159. Link: https://bit.ly/2ZRTNJI
- Dutta HK (2016) Cervical ganglioneuroma in a child. SM J Pediatr Surg 2: 1013. Link: https://bit.ly/2JegeC7
- Urata S, Yoshida M, Ebihara Y, Asakage T (2013) Surgical management of a giant cervical ganglioneuroma. Auris Nasus Larynx: 577-580. Link: https://bit.ly/2YgkB6b
- Lima AF, Moreira FC, Menezes A, Dias L (2018) Cervical ganglioneuroma in pediatric age: a cese report. Turk Arch Otorhinolaryngol 56: 237-240. Link: https://bit.ly/31W8eyw
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.



 Save to Mendeley
Save to Mendeley
