Archives of Otolaryngology and Rhinology
Solitary Plasmacytoma of bilateral temporal bone in a patient with multiple myeloma
Nouf Albakheet1*, Elaf Essa Ahmed2, Yazeed Al-Shawi3 and Khabti Almuhanna4
2Senior Resident, Prince Sultan Medical Military City, Riyadh KSA, Saudi Arabia
3Otology\Neurotolgy fellow at King Abdullah Ear Specialist Center, and senior registrar at Prince Sultan Medical Military City, Riyadh, Saudi Arabia
4Consultant Otorhinolaryngology, Subspecialty Otology and Cochlear Implant at Prince Sultan Military Medical City, Riyadh KSA, Saudi Arabia
Cite this as
Albakheet N, Ahmed EE, Shawi YA, Almuhanna K (2019) Solitary Plasmacytoma of bilateral temporal bone in a patient with multiple myeloma. Arch Otolaryngol Rhinol 5(4): 111-113. DOI: 10.17352/2455-1759.000111Introduction: Plasmacytomas are tumors that results from monoclonal proliferation of plasma cells. Disseminated form is called Multiple Myeloma (MM) which is characterized by multiple lytic bone lesions on imaging and monoclonal gammopathy.
Case presentation: A 53-year-old male presented to the emergency department with post auricular swelling in the right side. Thorough history and examination of the patient were done. Laboratory investigations, bone biopsy, and imaging of the patient were all consistent with MM and Solitary Plasmacytoma of Bone (SPB). The patient was started on chemotherapy and showed regression of the swelling.
Discussion: SPB is a subtype of plasmacytoma. SPB represents less than 5% of plasma cell tumors. SPB can occur in various locations, but temporal bone involvement is considered rare. There is strong association between SPB and MM in which almost half of patients presenting with SPB will have a pre-existing MM and more than 75% of patients with SPB will progress to MM.
Conclusion: Surgeons should keep the SPB as one of the differential diagnosis when they encounter such a presentation since it is a rare diagnosis.
Introduction
Plasmacytomas are tumors that results from monoclonal proliferation of plasma cells. They are subdivided into two subtypes based on their origin into Solitary Plasmacytoma of Bone (SPB) and Extramedullary Plasmacytoma (EP) [1]. SPB arises intramedullary and shows bone erosions. Disseminated form is called Multiple Myeloma (MM) which is characterized by multiple lytic bone lesions on imaging and monoclonal gammopathy. In the head and neck, SBP are considered rare malignancies [2]. Here we present a case of bilateral SPB in a 53 years old patient who is a known case of MM.
Case Presentation
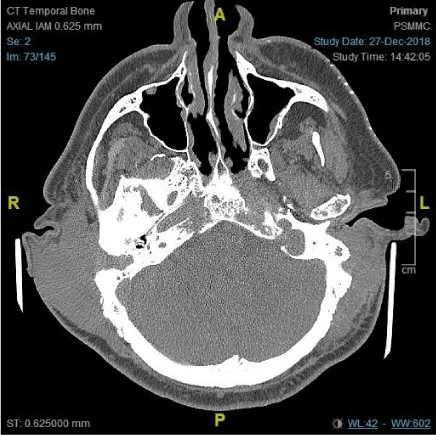
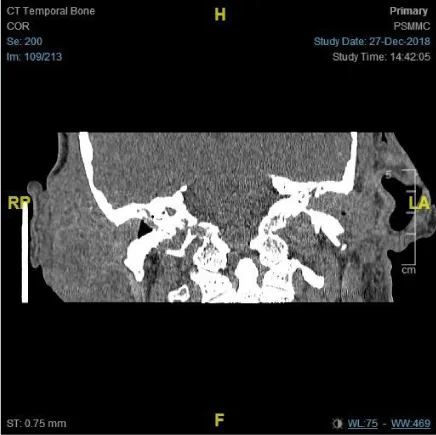
A 53-year-old male presented to the emergency room with three months of progressive swelling in the right post auricular region. The patient is a known case of diabetes mellitus, benign prostatic hyperplasia, hypertension, chronic kidney disease. Patient is on oral hypoglycemic medication and insulin, and he is a smoker. He was also just worked up for multiply spinal lytic lesions which came to be multiple myeloma. The examination showed tender, warm, soft, non-fluctuating right post auricular swelling measuring 3×8cm (Figure 1). There was a smaller swelling noted in left postauricular area measuring 1×1cm. Complete blood count with differentials showed the following results WBC: 9.4(n 4-11×10^9/1); Hb: 9.4 (12.5-18g/d1); PLT: 96(n 150-450 10^9/1); Neutrophils 74. Peripheral blood smear showed Red Blood Cells (RBC) with rouleaux formation with few normal RBCs, and thrombocytopenia was confirmed. The patient was given Vancomycin and Ceftriaxone and got admitted to the hospital. A trail of aspiration was done and showed no pus collection. Computed Tomography (CT) imaging of the temporal bone was done without contrast due to patient’s kidney condition, and the showed bilateral destructive masses in the temporal area (Figure 2). A whole-body Positron Emission Tomography (PET) scan showed multiple metabolic active hypo-dense osteo-medullary lesion consistent with multiple myeloma. FNA from right swelling was taken which showed plasma cells. Bone marrow biopsy was consistent with plasma cell myeloma in which it showed hypercellularity (100%) due to infiltration by plasma cells accompanied by fibrosis grade 3 by reticulin stain. Immunohistochemistry stains of the malignant cells showed lambda light chains, CD138, and CD79a. The patient was presented in tumor board meeting and he was started on bortezomib (targeted therapy) and dexamethasone according to hospital chemotherapy protocol. Patient was also covered with antibiotics during the chemotherapy course as prophylactic and for the mild cellulitis noticed over the swelling. On following up the patient, regression in the swelling size was noticed few weeks after starting chemotherapy treatment (Figure 3). Two months later, the swelling almost resolved (Figure 4).
Discussion
SPB represents less than 5% of plasma cell tumors [5]. SPB can occur in various locations with the vertebral bodies and ribs being the most common sites. Temporal bone involvement is considered rare. It has been observed in the literature that the petrous apex is involved the most due to the relatively its high amount of marrow found there. However, other sites of temporal bone have been involved, and also there has not been any report in the literature of bilateral involvement of temporal bone; hence, this case is the first. There is strong association between SPB and MM in which almost half of patients presenting with SPB will have a pre-existing MM, and more than 75% of patients with SPB will progress to MM. The average age of patients presenting with SPB is between 50–70 years with male predominance. Presentation of SBP in nonspecific and tends to mimic other benign and malignant lesion that commonly encountered in the temporal bone. Neurologic examination is thought to be indispensable to look for cranial nerve involvement [3-5].
Plasmacytoma histologically appears as sheets of plasma cell with different degrees of atypia. Immunophenotyping to the plasmacytoma will show light chains [4]. Radiologically, plasmacytoma can appear as lytic or multicyclic lesion. on CT, plasmacytoma gives an iso-intense appearance on T1 images and hyperintense appearance on T2 images [2]. T2 wighted MRI allows the distinction between the tumor and fluid and make it appears as hypointense, and the mass becomes homogenous with contrast infusion [6].
SPB is radiosensitive, hence, the standard of care is local radiation therapy with doses of 40000-5000 Gray administered daily. This has resulted in 83%-96% local control rate. The role of adjuvant chemotherapy in SPB is not clear, however, it has been proposed that it can help in the prevention or the delay of progression to MM. In this case, bilateral SPB responded well to chemotherapy alone as part of MM management. Surgical resection is not feasible in some cranial locations and indicated in cases of neurological and surgical instabilities. Following up patient to assess the response rate is accomplished through obtaining monoclonal protein levels and assessing the regression or progression of the evident signs and symptoms along with the lesions on imaging [5].
Conclusion
SPB is a subtype of plasmacytoma that arises intramedullary and shows bone erosions. It is diagnosed through radiographic and histologic means. Radiation therapy is the standard of care for management of SPB. However, our case was managed through chemotherapy. All in all, surgeons should keep the SPB as one of the differential diagnosis when they encounter such a presentation since it is a rare diagnosis.
- Chiang SK, Canalis RF, Ishiyama A, Eversole LR, Becker DP (1998) Plasmacytoma of the temporal bone. Am J Otolaryngol 19: 267-273. Link: http://bit.ly/34wVhM0
- Jun HJ, Choi J, Kim KM, Chae SW (2013) Multiple Myeloma With Isolated Plasmacytoma in Temporal Bone. Otol Neurotol 34: e107–e108. Link: http://bit.ly/2WGB5EI
- Engelsma RJ, De Bree R, Janssen JJ, Scheeren RA (2000) Plasmacytoma of the mastoid bone: solitary and systemic. J Laryngol Otol 114: 378-380. Link: http://bit.ly/2qjq00j
- Sweeney AD, Hunter JB, Rajkumar SV, Lane JI, Jevremovic D, et al. (2017) Plasmacytoma of the Temporal Bone, a Great Imitator: Report of Seven Cases and Comprehensive Review of the Literature. Otol Neurotol 38: 400-407. Link: http://bit.ly/36Cbv8c
- Kumar R, Kumar N, Mohindro S, Radotra BD (2017) Solitary plasmacytoma of temporal bone: A rare case report. Asian J Neurosurg 12: 95-97. Link: http://bit.ly/2rglfVJ
- George JC, Caldemeyer KS, Kreipke DL, Chalian AA, Moran CC (1994) Solitary plasmacytoma of the mastoid bone presenting as coalescent mastoiditis. Arch Otolaryngol Head Neck Surg 120: 1393-1394. Link: http://bit.ly/2ND4Sdg
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.




 Save to Mendeley
Save to Mendeley
