Archives of Otolaryngology and Rhinology
Bilateral Intraoral Mucosal Flaps for Repair of Vestibular Stenosis Following Rhinoplasty & Airway Reconstruction: A Case Report
Brian P Dickinson1,2*, Monica Vu1 and Nikkie Vu-Huynh1
2Hoag Memorial Hospital Presbyterian, USA
Cite this as
Dickinson BP, Vu M, Huynh NV (2020) Bilateral Intraoral Mucosal Flaps for Repair of Vestibular Stenosis Following Rhinoplasty & Airway Reconstruction: A Case Report. Arch Otolaryngol Rhinol 6(2): 037-040. DOI: 10.17352/2455-1759.000119Background: Aesthetic rhinoplasty is a challenging specialty for surgeons as both the demands of patients and physicians are high. Preservation rhinoplasty brings many advances and advantages to the rhinoplasty with the intent of decreasing the need for revision or secondary rhinoplasty through change that is less destructive. Nonetheless, there are often patients in the rhinoplasty surgeon’s practice who have either aesthetic or functional sequelae from previous open or more reduction-oriented procedures. One of the more troublesome complications for the patient to live with, and the surgeon to correct, is vestibular stenosis.
Purpose: To present a simple method and technique for repairing vestibular stenosis that is easily reproducible. We present a technique previously described for repair of cleft-lip and palate rhinoplasty sequelae, but not frequently utilized in the aesthetic rhinoplasty population. This technique is within the same operative field and does not require additional cartilage grafts.
Method/Results: A 25 year old female Middle Eastern patient underwent septorhinoplasty to reduce the size of her nose and improve breathing. The patient underwent a revision operation to further reduce her nose and with the addition of nostril sill excisions. The patient did well post-operatively, but eventually developed difficulty breathing and bilateral circumferential webs of the nasal vestibule. This was corrected with bilateral, medially-based 1.5cm width and 3cm length intraoral mucosal flaps to the nostril sill and the floor of the nasal airway. The flaps were inset with 4.0 chromic suture, and the intraoral harvest site was closed with chromic suture. The nose was then stented with Doyle splints bilaterally. The patient started hyperbaric oxygen therapy 1 day post-operatively and received 5 consecutive treatments in total.
Conclusion: From a functional and aesthetic standpoint, cicatricial vestibular stenosis following aesthetic rhinoplasty is a challenging problem to correct. The intraoral mucosal flap offers a viable option which is easily reproducible and is within the same operative field. Hyperbaric oxygen therapy is a useful adjunct for flap viability.
Introduction
Vestibular stenosis of the nasal airway is a challenging problem for both the nasal surgeon and the patient [1-4]. Typically, a repair of vestibular stenosis is the result of previous trauma, burn, or congenital cleft lip and palate [5-8]. These stenotic vestibular wound beds are frequently associated with significant scarring. In order to repair these defects, either vascular lining and/or structural support is necessary to prevent scar contracture from recurring [2-8]. Additional donor sites are often more accepted by patients who have undergone previous procedures where donor tissue has already been borrowed to correct sequelae of their disease process.
Aesthetic rhinoplasty is a challenging and very humbling specialty as both the demands and expectations of patients and physicians are high. The field of rhinoplasty continues to evolve. Preservation rhinoplasty now utilizes techniques without the removal of cartilage and maintains subchondral planes with the intention of preventing unwanted or unpredictable scarring of the external or internal nose.[1] Before the advent of preservation rhinoplasty, creating a smaller nose relied on aggressive reduction rhinoplasty techniques. These aggressive reductions have the potential for more scarring and possibly obstructing the airway. We present here a simple method to repair bilateral vestibular stenosis following cosmetic rhinoplasty using a cleft rhinoplasty repair technique. The technique is not frequently used in the aesthetic rhinoplasty population, but is easily reproducible and safe.
Methods
A photographic chart review was conducted on a patient who iatrogenically acquired bilateral vestibular stenosis after a revision rhinoplasty and airway operation. The intraoperative photographs were analyzed and placed into a step-by-step method to repair vestibular stenosis in the aesthetic rhinoplasty and airway patient.
Results
A 25-year-old Middle Eastern female patient wished to have a smaller nose and underwent septorhinoplasty. The patient healed well, but returned with a complaint that the nasal tip was droopy and desiring an even smaller nose. In a second revision operation, the lower lateral cartilages were cephalically rotated with both a tip rotation suture and tongue in groove technique, and a nostril sill excision was conducted. The patient was happy with the aesthetic result, but returned several months later with bilateral airway obstruction worse than the symptoms of the deviated septum [Figure 1].
To limit more manipulation of the nasal airway and additional scarring without the need for additional grafts, we utilized a cleft rhinoplasty technique from the oral mucosa to repair the bilateral vestibular stenosis. The figures most appropriately explain the markings and technique for repair. The patient was brought to the operating room under general anesthesia and the following steps were taken:
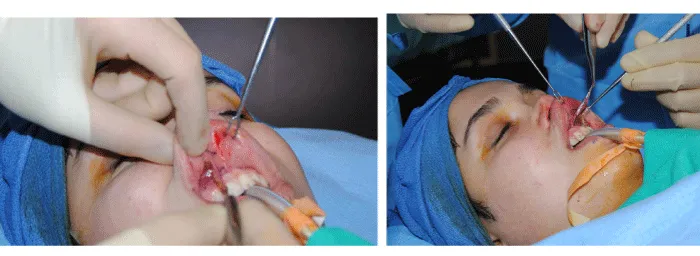
Step 1: The nose and maxillary oral mucosa were injected with 0.25% marcaine with epinephrine for anesthetic and hemostatic control [Figure 2].
Step 2: An incision was made along the floor of the nose with a number 15 blade scalpel. A nasal speculum was then inserted to dilate the floor of the nose and create a floor of nose defect [Figure 3]. The width of the defect created was measured with calipers.
Step 3: Double hooks were placed in the upper lip to expose the oral mucosa. Bilaterally, a medially based oral mucosal flap was drawn stopping within 1 cm from the upper lip frenulum.
The width of the mucosal flap drawn was wider than the defect created into the nose [Figure 4].
Step 4: The mucosal flaps were then incised with Bovie electrocautery on cut and incised using full thickness mucosa [Figure 5].
Step 5: Tunnels were then created from the oral side to the nasal side using mosquito clamps to protect the mucosal flap from being damaged [Figure 6].
Step 6: One the tunnel was safely created, the mosquito clamp was then passed from the nose to the mouth to grasp the mucosal flap and deliver it into the nose [Figure 7].
Step 7: The oral mucosal flap once delivered, was then inset in the floor of the nose. The freely mobile end of the mucosal flap was placed most posteriorly in the nose and sutured with a 4.0 chromic suture [Figure 8].
Step 8: Doyle splints were then sutured into the nose using chromic suture to serve as a bolster for the graft and prevent motion [Figure 9].
The patient was given Keflex for 5 days postoperatively for surgical prophylaxis. Hyperbaric oxygen therapy was initiated on post-operative day one and the patient received 5 treatments of one hour duration. The Doyle nasal stents remained in place for three days postoperatively prior to being removed. The patient was instructed to wear nasal stents for the remaining 11 days day and night. After that the nasa stents were worn nightly for one month. The patient was seen post-operatively once a week for six weeks.
Discussion
Aesthetic surgery of the nose can be one of the more difficult and humbling operations for plastic surgeons and head and neck surgeons. Patients have often invested a significant amount of money and time off from work to undergo their operation.When the operation goes well, it can be extremely satisfying for the patient and the operating surgeon. When the operation results in an airway compromise, or the results change negatively over time, it can cause a significant amount of frustration and for both parties. As a rhinoplasty surgeon works toward making the nose smaller there may also be an increase in post-op nasal airway obstruction. Revision or secondary procedures with rib cartilage or other grafts often necessitates opening the nose with more undermining and exposure. This usually comes with another round of significant swelling, and healing process for the patient. Often, in the secondarily obstructed patient, the patient already approves of their aesthetic improvement but only desires to correct the stenosis to improve their breathing.
The concept of preservation rhinoplasty has evolved with the intention of decreasing the need for revision or secondary operations by preserving structure [1]. When revisions are needed, they can be accomplished in a separate plane and with more ease of dissection. The revision operation in our patient resulted in significant scarring and the resulting vestibular stenosis. Overtime and after reading about vestibular stenosis, we understood that the problem is not always related to support, but rather the forces of scar contracture on a “weaker” cartilage construct [2-8].
The technique presented is a cleft rhinoplasty technique which can be accomplished in a small amount of time with a minimal amount of healing and swelling. The technique does not require re-opening the nose, which would risk the possibility of damaging the already weak lower lateral cartilages. It also does not require dissection to create nasal mucosal flaps to nourish cartilage grafts, which may not survive in the scarred nose or possibly obstruct the nose even more. This technique can be helpful in the re-operative aesthetic patient who has an acceptable aesthetic result and would like an improvement in the airway.
Conclusion
Aesthetic and airway surgery of the nose can be very rewarding and humbling at the same time. Planning surgery with the intention to help patients understand the process and the possibility of airway obstruction late post-operatively is prudent. Preservation rhinoplasty techniques seem promising to reduce unpredictable scarring. An understanding of a few techniques to repair vestibular stenosis can be helpful to the young rhinoplasty surgeon early in practice.
- Daniel RK (2018) The Preservation Rhinoplasty: A New Rhinoplasty Revolution. Aesthet Surg J 38: 228-229. Link: https://bit.ly/3caCBpA
- Menger D, Lohuis PJFM, Kerssemakers S, Trenité GJN (2005) Postoperative Management of Nasal Vestibular Stenosis: The Custom-made Vestibular Device. Arch Facial Plast Surg 7: 381-386. Link: https://bit.ly/2W9gdYb
- Yoon BW, Kim DW, Choi SJ, Cho KS (2018) Latrogenic nasal vestibular stenosis after maxillofacial reconstructive surgery. Braz J Otorhinolaryngol 84: 126-130. Link: https://bit.ly/2xIf3ta
- Gupta M, Rai AK (2008) Bilateral nasal vestibular stenosis: a case of rhinoscleroma and review of surgical techniques. Indian J Otolaryngol Head Neck Surg 60: 72-75. Link: https://bit.ly/3calnbD
- Daines SM, Hamilton GS, Mobley SR (2010) A graded approach to repairing the stenotic nasal vestibule. Arch Facial Plast Surg 12: 332-338. Link: https://bit.ly/2W6yzsI
- Aydogdu E, Akan M, Gideroglu K, Akoz T (2006) Alar transposition flap for stenosis of the nostril. Scand J Plast Reconstr Surg Hand Surg 40: 311-314. Link: https://bit.ly/3bb3IQ2
- Salvado AR, Wang MB (2008) Treatment of complete nasal vestibule stenosis with vestibular stents and mitomycin C. Otolaryngol Head Neck Surg 138: 795-796. Link: https://bit.ly/2SBgjFJ
- Kotzur A, Gubisch W, Meyer R (1999) Stenosis of the nasal vestibule and its treatment. Aesthetic Plast Surg 23: 86-92. Link: https://bit.ly/3dlNPHN
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.









 Save to Mendeley
Save to Mendeley
