Archives of Otolaryngology and Rhinology
A Step-by-Step Approach to Free Fibula Flap Mandible Reconstruction of Mandibular Pathologic Fractures: A Pictorial Essay
Brian P Dickinson1-3*, Nikkie Vu-Huynh1, Monica B Vu1, Amy Tsai1, Timothy Kelley2, George Semeniuk2, Brian Kim2, Craig Cox2 and Peter Ashjian2-4
2Hoag Memorial Hospital Presbyterian, Newport Beach, CA, USA
3Adventist Health Glendale, Glendale, CA, USA
4M.D., Inc.. Glendale, CA, USA
Cite this as
Dickinson BP, Huynh NV, Vu MB, Tsai A, Ashjian P, et al. (2020) A Step-by-Step Approach to Free Fibula Flap Mandible Reconstruction of Mandibular Pathologic Fractures: A Pictorial Essay. Arch Otolaryngol Rhinol 6(2): 052-057. DOI: 10.17352/2455-1759.000122Background: Pathologic fractures of the mandible following radiation and embolization can be a challenging problem for patients. Occasionally, patients have already completed the oncologic component of their treatment and are trying to move on with their lives. A pathologic fracture is not only painful, but also a frustrating hindrance as it limits food intake and overall nutrition. In addition, pathologic fractures are challenging to repair.
Purpose: To demonstrate a step-by-step approach for pathologic mandibular fracture repair with an ipsilateral free fibula flap following oncologic resection of a tonsillar tumor that underwent pre-operative embolization and post-operative radiation therapy.
Methods/Results: A 65 year old male presented with a tonsillar head and neck tumor. The patient had pre-operative embolization for an intra-oral bleed, successful resection with clear margins, and then post-operative radiation therapy. During a subsequent dental procedure, the patient developed a pathologic mandibular fracture with subsequent pain and malocclusion including a posterior open bite. The pathologic mandible fracture was repaired with and ipsilateral free fibula flap. A chart review was completed to create a pictorial essay to describe our technique.
Conclusion: Successful repair of pathologic mandibular fractures can be rewarding for the operative surgeon and satisfying for the patient. Optimizing chances of success are improved with pre-operative CT scans and orthodontic models as well as intra-operative models. A step by step intraoperative approach is helpful for maximizing success and optimizing occlusion.
Introduction
-->Pathologic fractures of the mandible are rare [1-5]. Defined methodology on how to treat them is not standard [1,4,6-8]. Repair of bone or soft tissue following radiation and osteoradionecrosis are challenging problems. Not only are tissues more hostile and blood supply compromised, but risk of infection and post-operative complications are more likely. The social challenges are heightened as well. Patients have completed successful surgical excision, chemotherapy, and radiation. They have thankfully resumed a “normal” life and can be frustrated with the introduction of a setback. Treatment of pathologic fractures of the mandible from osteoradionecrosis varies on age and overall medical health of the patient [4,8]. In the young healthy patient, adequate treatment can include resection of the osteoradionecrosis segment and replacing it with a vascularized bone graft. This requires additional surgery and often a gastrostomy tube and tracheostomy to protect the repair and for safety.
When head & neck, and plastic & reconstructive surgeons are in practice early on, they are presented with many difficult cases. This reconstruction is particularly complicated as it is important to retain the functional teeth, maintain the patient’s occlusion, and construct a fibula flap that is small enough to be inset to fill the resulting defect of the resection. While larger tumors or resections require larger bone grafts, the smaller segments of bone are removed to retain functional teeth. Given the rarity of pathologic fractures and their treatment, it is hard to find a solution to approach this scenario in a textbook; and operating without planning can lead to the pitfall of post-operative malocclusion. Repairing pathologic fractures in the radiated and embolized setting is not straightforward and should be accomplished carefully. The pathologic malocclusion first requires establishing appropriate dental occlusion, followed by surgical resection, and finally, free vascularized tissue as the surrounding tissue is hostile to other methods. We present a step-by-step approach to this difficult problem so that Head & Neck or Plastic & Reconstructive surgeons can use it as a reference when trying to manage these surgical problems.
Methods
A photographic chart review was conducted on our patient who developed a pathologic fracture of the mandible after a prior history of successful tonsillar cancer treatment. The 65 year old male patient had preoperative embolization for an intra-oral bleed, successful tonsillar resection with clear margins, and then postoperative radiation therapy. During a subsequent dental procedure, over one year after radiation therapy, the patient developed a pathologic mandibular fracture with subsequent pain and malocclusion including a posterior open bite.
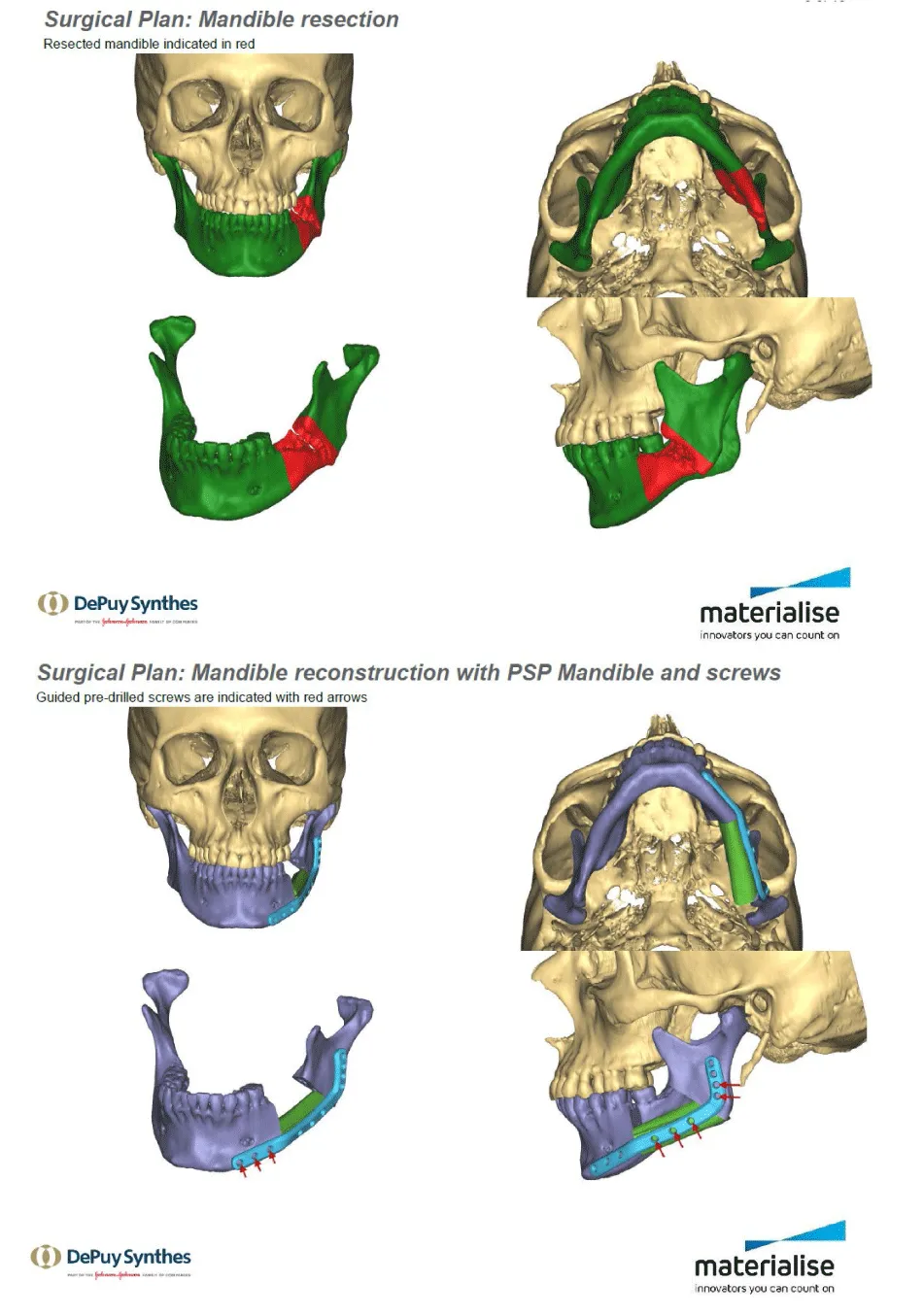
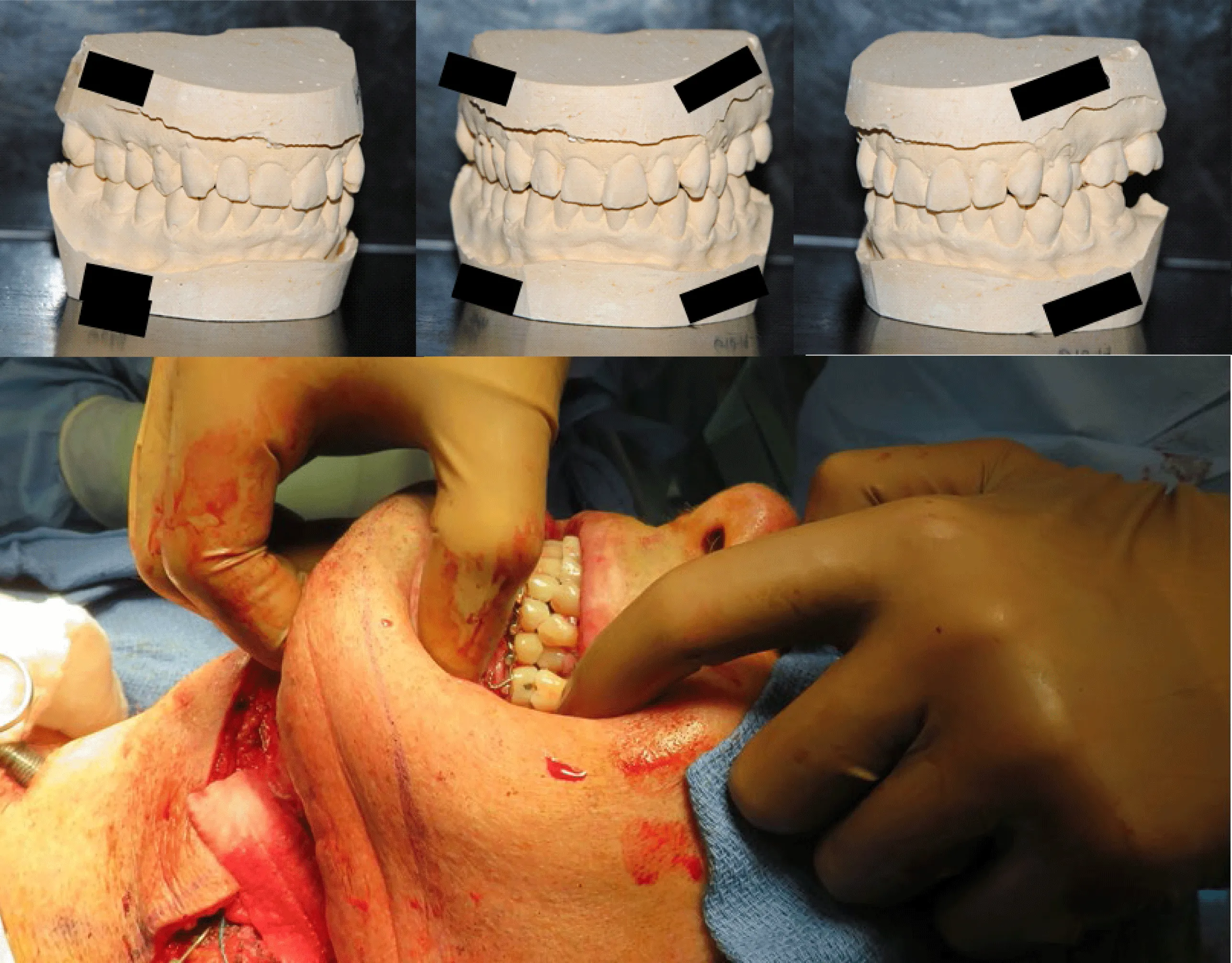
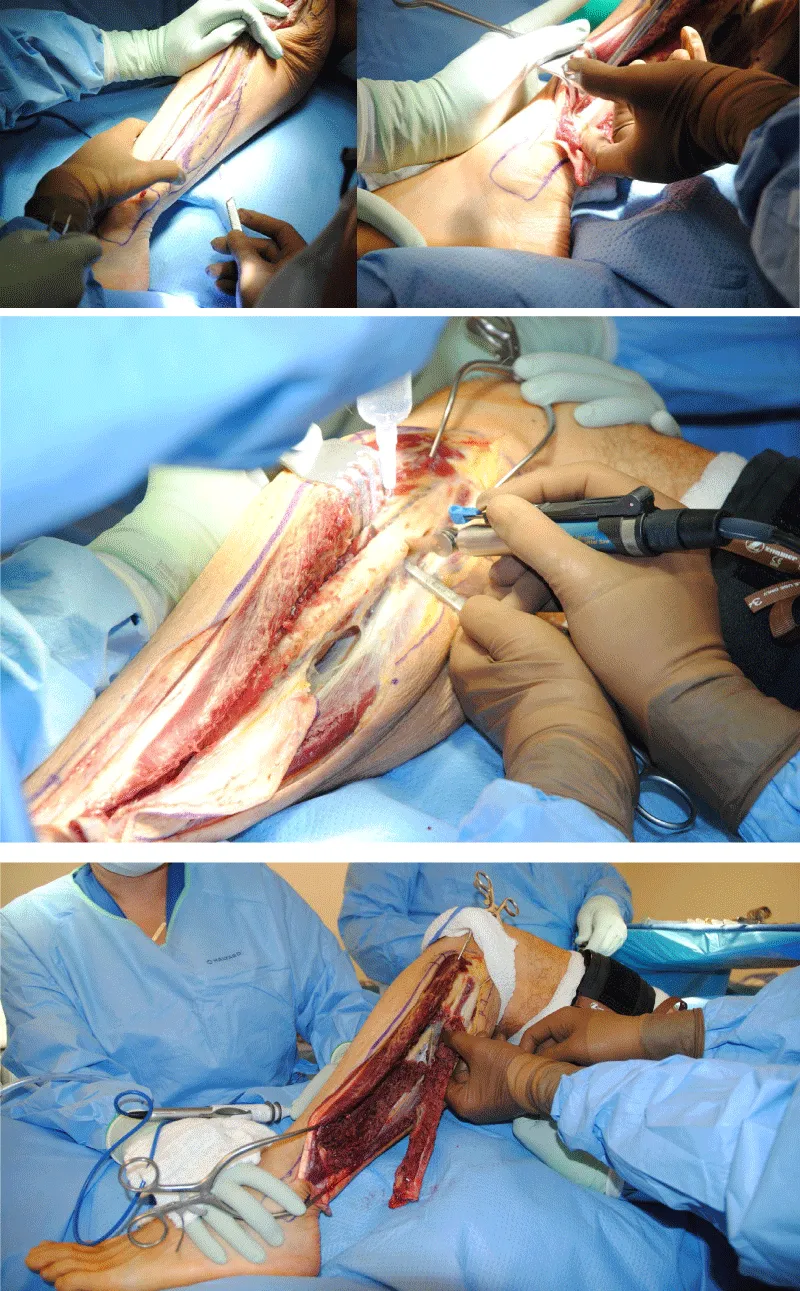
A panorex, as well as a pre-operative anatomic fine-cut CT-scan of the face/mandible, was obtained. The estimated bone resection of the pathologic fracture was 4 cm. Given the previous embolization and radiation therapy, vascularized fibula was selected for autologous reconstruction. Dental models of the maxillary and mandibular teeth were obtained from the patient’s dentist to better understand the occlusal alignment. Synthes intra-operative models and occlusal splints were created to facilitate occlusal alignment. Photographs obtained intra-operatively as well as photos of the pre-operative plan were used to develop a step-by-step approach for head & neck and plastic & reconstructive surgeons to use as a surgical flight plan.
Adjunctive treatments include G-tube placement for nutrition while awaiting intraoral wound closure, hyperbaric oxygen therapy for facilitating healing in the radiated bed, and Head & Neck occupational therapy for relieving jaw stiffness.
Results
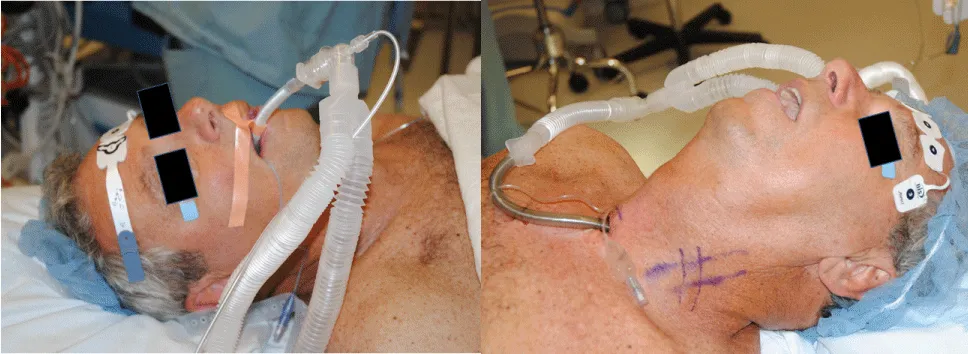
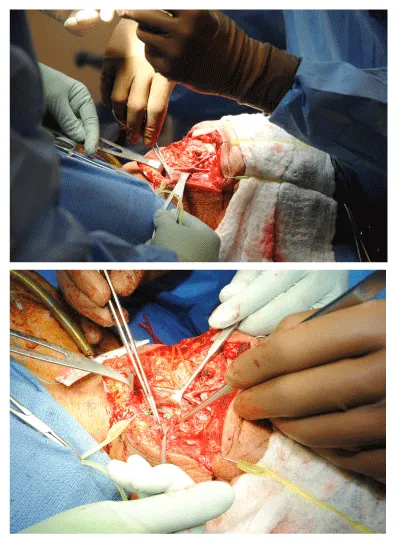
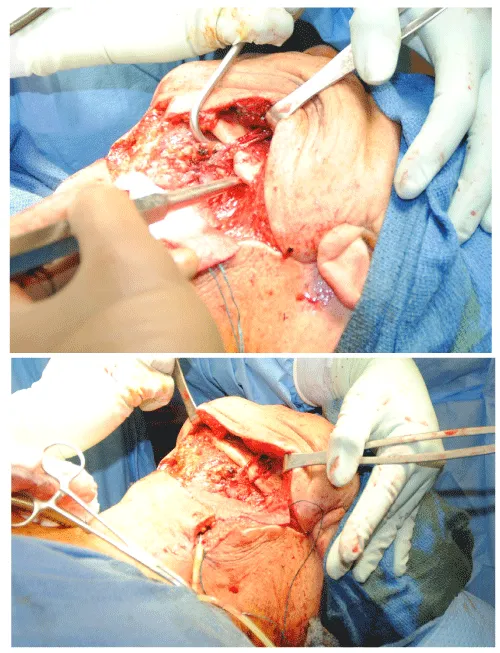
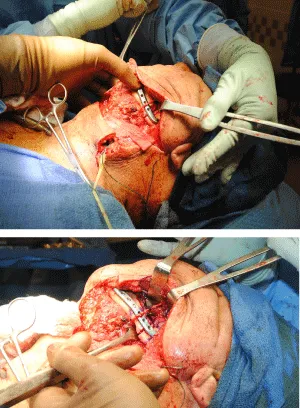
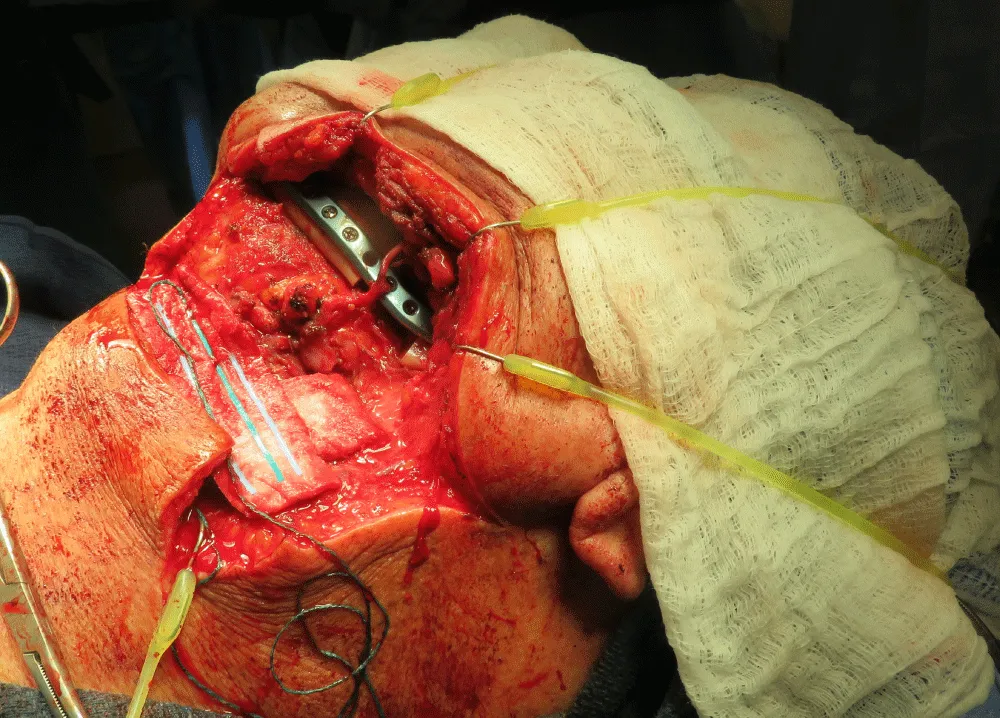
The appropriate medical clearance was achieved. The patient was taken to the operating room, and the surgical flight plan created was followed with photographs of the representative steps of the operation (Figures 1-16).
Discussion
Pathologic fractures of the mandible occur infrequently, and the surgical management will depend on the etiology of the fracture and the patient. The treatment of these fractures and their repair are technically challenging but rewarding for the operating team and the patient. In our patient, the malocclusion and the pain were the operative indications for surgical resection and reconstruction. In the re-operative patient, we have found that taking necessary precautions in all steps of the planning is helpful to maximize outcome. Often in the re-operative and frustrated patient, there is an overtone of trying to appease the patient and not cause further inconvenience. In our experience, it is important not to omit any standard pre-operative or operative steps to placate the patient despite their frustration. Reiterating to the patient that measures such as gastrostomy tube, tracheostomy, etc. are needed for safety will help the re-operative patient to understand. It is important to reiterate the success of their cancer treatment.
The impetus for this article was to create a step-by-step approach to mandibular resection and reconstruction in the patient with pathologic fracture so that when we, or other head & neck or plastic & reconstructive surgeons encounter a similar patient scenario, they can follow this guideline in a easily reproducible manner. The techniques themselves are not novel or unique, but rather involve steps from different procedures combined into one. What is important about the pathologic fracture reconstruction is that the occlusion is not normal to begin with. Unlike a traditional resection and reconstruction, the occlusion is often normal or normal enough to be maintained. In our patient it was important to first to recreate and mobilize the fracture and re-establish occlusion before embarking on resection and reconstruction.
In the patient who had previous embolization and previous surgery and radiation, we find that a pre-operative ultrasound of the neck to look for arterial and venous recipient vessels is helpful. The vascular ultrasound can not only detect flow, but also diameters of veins and arteries to help select larger diameter vessels or select for favorable size matching. In this patient, the facial artery underwent preoperative embolization as the patient had experienced bleeding. Although we dissected out the facial artery, the presence of a coil and absence of flow made it unusable for anastomosis. The superior thyroid was dissected out and utilized. The diameter of the superior thyroid vessels was small, but the size matched favorably when anastomosed to the peroneal artery. An important step order is to make sure the recipient vessels are available prior to the osteotomies. If recipients are not available, alternative options need to be considered.
Conclusion
Head & neck reconstruction is a challenging and humbling field of surgery, but nonetheless rewarding. This surgical case encompasses many different surgical principles, the most important are surgical planning and safety. In early stages of one’s career, it is helpful to maintain a photo journal of maneuvers performed. This can help for future cases the surgeon encounters and serve as a measure for improvement in outcomes, efficiency, and to minimize complications.
- Boffano P, Roccia F, Gallesio C, Berrone S (2013) Pathological mandibular fractures: a review of the literature of the last two decades. Dent Traumatol 29: 185-196. Link: https://bit.ly/2M3XO9f
- Gerhards F, Kuffner HD, Wagner W (1998) Pathological fractures of the mandible. A review of the etiology and treatment. Int J Oral Maxillofac Surg 27: 186-190. Link: https://bit.ly/2AbE7K1
- Grau-Manclús V, Gargallo-Albiol J, Almendros-Marqués N, Gay-Escoda C (2011) Mandibular fractures related to the surgical extraction of impacted lower third molars: a report of 11 cases. J Oral Maxillofac Surg 69: 1286-1290. Link: https://bit.ly/2zyCmGK
- Boffano P, Roccia F, Gallesio C, Demo PG, Guglielmo R (2012) Surgical Management of Pathologic Mandibular Fractures. J Craniofac Surg 23: e560-e562. Link: https://bit.ly/2ZRwNy3
- O’Brien DC, Jones G, Yell M, McChesney J (2018) Case Report and Literature Review of a Pathologic Mandibular Fracture from Metastatic Esophageal Adenocarcinoma. Case Rep Otolaryngol 2018. Link: https://bit.ly/3ere28j
- Zhao Y, Li RF, Sun YF, Liu B, Jia J (2017) Pathological Fractures of the Mandible: A Report of 27 Cases. Clin Surg 2: 1839. Link: https://bit.ly/36vhagX
- Noriaki A, Arisa I, Yasufumi K, Koyama C, Iida M, et al. (2017) Pathological Fracture Successfully Treated with Simple Orthodontic Appliance, Chin Cup after Cyst Removal. J Dent Oral Disord Ther 5: 1-4. Link: https://bit.ly/2M21YhL
- Kim C, Park M, Yun S, Kim JW (2015) Treatment of pathologic fracture following postoperative radiation therapy: clinical study. Maxillofac Plast Reconstr Surg 37: 31. Link: https://bit.ly/2X7kiwu
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.









 Save to Mendeley
Save to Mendeley
