Archives of Otolaryngology and Rhinology
Use of ureteral catheter for under vision suctioning in rigid therapeutic bronchoscopy in children: A novel approach
Krushnakumar V Kesan1*, Sikha K Kesan2, Arvind Ade3 and Paras Kothari4
2Director, Kesan Hospital, Akola, Maharashtra, India
3MS surgery, Professor and Head, Department of Surgery, Govt Medical College, Akola, Maharashtra, India
4MCh Pediatric surgery, Professor and Head of the Department, Department of Pediatric Surgery, LTMMC & LTMGH Sion, Mumbai, India
Cite this as
Kesan KV, Kesan SK, Ade A, Kothari P (2020) “Use of ureteral catheter for under vision suctioning in rigid therapeutic bronchoscopy in children: A novel approach”. Arch Otolaryngol Rhinol 6(3): 071-075. DOI: 10.17352/2455-1759.000126Background: Rigid bronchoscopy is a common procedure and treatment of choice for foreign body (FB) in respiratory tract. Blind suctioning using rigid suction cannula is associated with technical difficulties and complications. Under vision flexible cannula are expensive and not commonly available. This led us to discover the alternative of using Ureteral catheters flexible suction cannula for under vision suctioning.
Patients and methods: A retrospective study was conducted in the department of Surgery at tertiary hospitals, from January 2015 to March 2020. Medical records and operative videos were analyzed. Forty two Paediatric patients with foreign body in respiratory tractwere subjected to rigid bronchoscopy and Ureteral catheterwas used as flexible suction cannula for under vision suctioning.
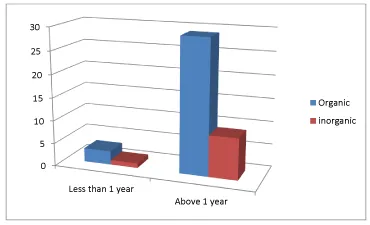
Results: Forty two patients (12 infants, 30 between age 1to 8 year; 26 males and 16 females) with FB bronchus subjected to rigid bronchoscopy. N = 32 were having organic FB and n = 10 were having inorganic (Graph 1), duration of FB in Respiratory tract ranged from 6 hours to 8 months, 7 in main bronchus, 33 having unilateral and 2 having Bilateral FB. Operative time ranged from 15 minutes to 75 minutes. 4 patients had slight intraoperative bleed due to mucosal injury, postoperative stay ranged from 1 to 4 days.
Conclusion: Use of Ureteral catheterfor under vision suctioning in rigid bronchoscopy in children quite feasible and effective technique. The main advantages in are simplicity, short operative time, Less traumatic, Good vision, with minimal complications.
Type of study: Treatment Study.
Level of evidence: LEVEL IV, Case series with no comparison group.
Introduction
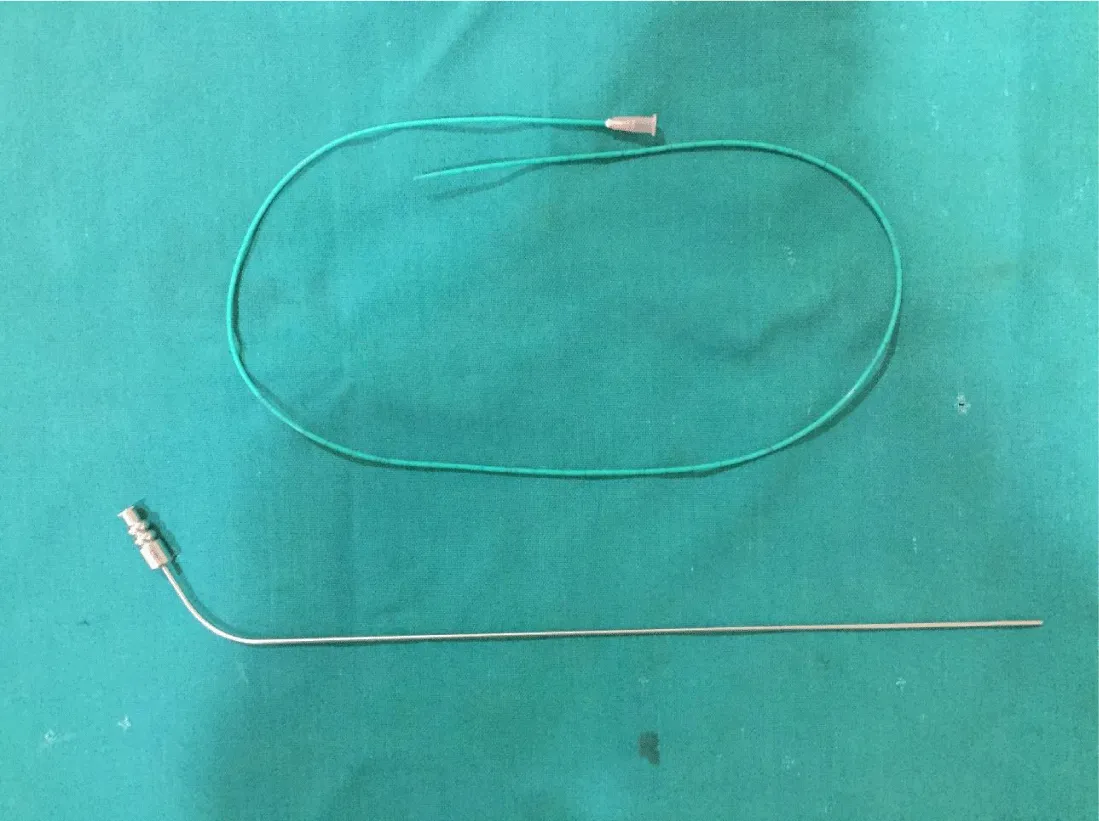
Foreign Body Aspirations (FBA) represent one of the most frequent cases of acute respiratory insufficiency and accidental death in subjects of paediatric age [1]. Aspiration of foreign bodies is an important and preventable cause of mortality and morbidity in children, especially those less than 3 years of age. Rigid bronchoscopic foreign body removal is considered the gold standard procedure for foreign body aspiration [2-4]. Under vision suctioning is of primary importance especially in organic and long standing impacted FB. Various flexible compatible suction catheters that can be passed in 3,5 mm or 4,5 mm sheath are not widely available in rural India and are also costly. This led us to use Ureteral cathetersize 4 to 5 Fr with attachments to be used for under vision suctioning in bronchoscopy. As its been rightly said, “Necessity is the mother of invention”). No prior study has included any reference or suggested this kind of technique for under vision suctioning inbronchoscopic FB removal.
Patients and methods
A retrospective study was conducted at multiple centers in a small sub urban city of Maharashtra, India, from January 2015 to March 2020. Records of 42 patients were analyzed. These 42 patients were diagnosed with foreign body in respiratory tract, and weresubjected to rigid bronchoscopy and ureteral catheter was used for under vision suctioning through side channel [Figure 1].
The data analyzed included patient details, nature of FB, duration of aspiration of FB, operative time, number of attempts for grasping and removal of FB, intra and post-operative complications.
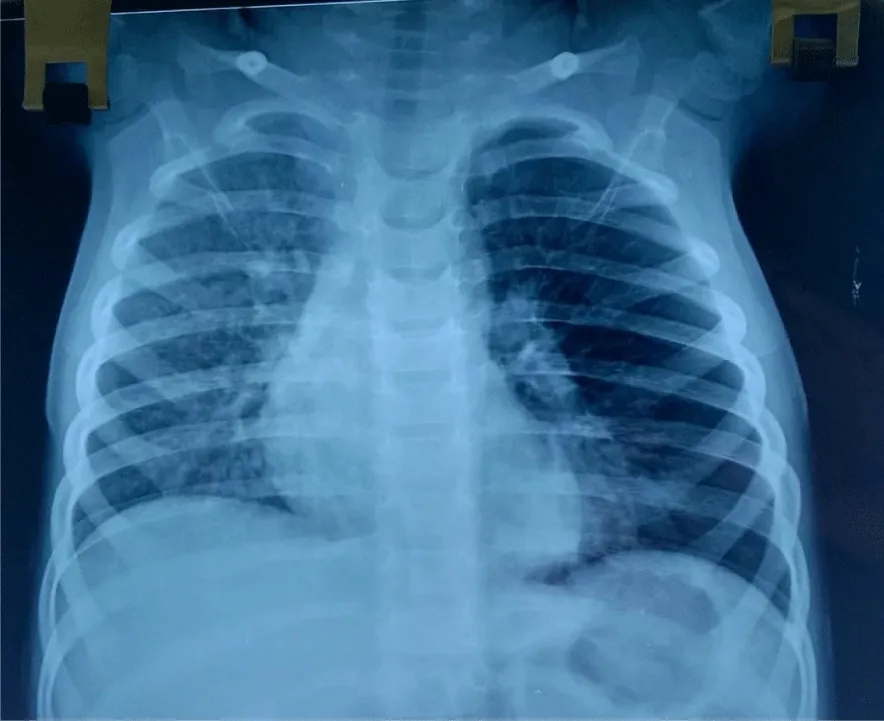
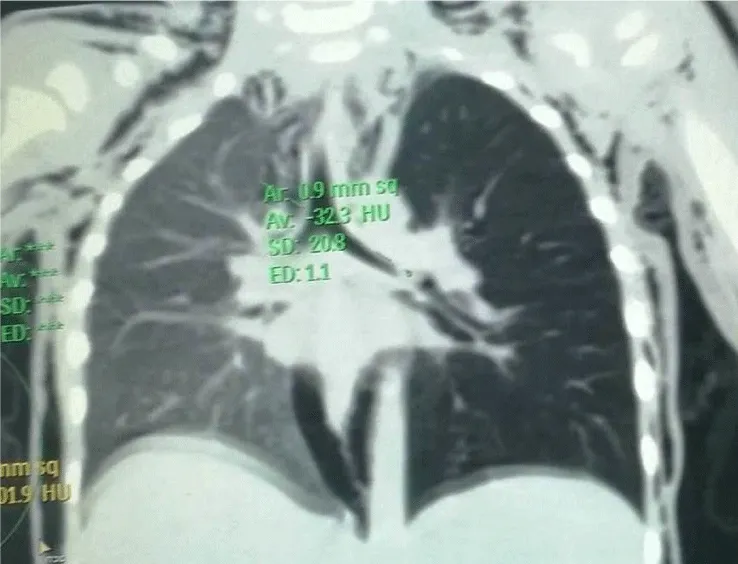
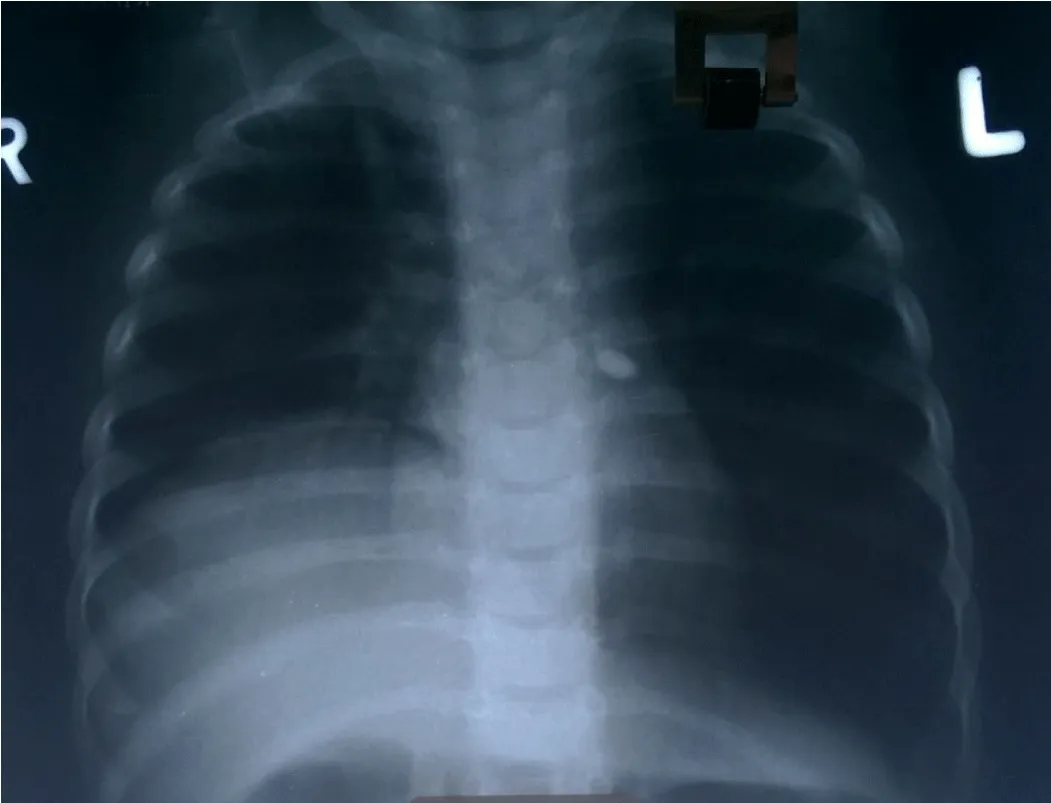
Diagnosis was made on history, x ray chest, fluoroscopy, few patients required CT thorax [Figures 2-4].
Following necessary preparation, ureteral catheter of size 4 or 5 Fr was used. Bronchoscope was assembled prior to induction of anesthesia with proper placement of screen (left side of patient if FB was in left bronchus; right in case of right bronchus; and at leg end in center if FB was in mainstream bronchus and in bilateral FB).
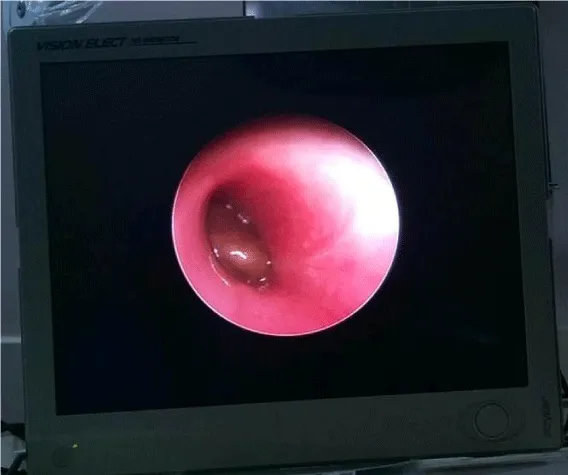
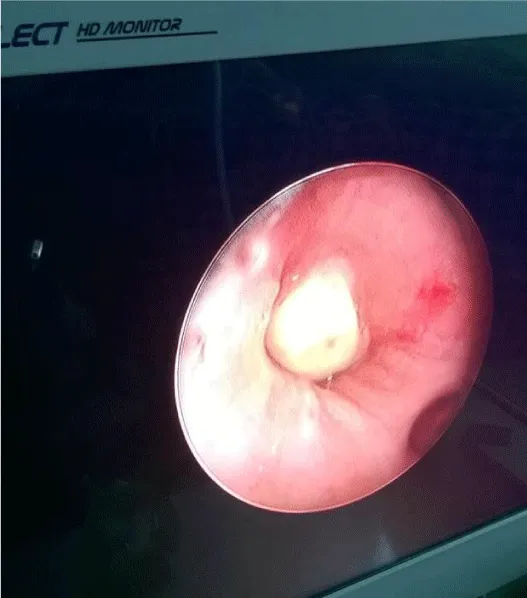
Patient was positioned supine with extended neck, boaster under the shoulder. Routine monitors and precordial stethoscope were attached. Topical lignocaine (10%) was sprayed over the laryngeal inlet. Under general anesthesia, rigid sheath of appropriate size ranging from 3,5mm to 4,5mm passed under vision using bridge by Paediatric surgeon. Assisted ventilation via the ventilating port was checked. Main and both bronchus were inspected for nature andlocation of FB (Figures 5,6). In case of long standing FB, or mucus or pus, if present around FB, especially organic FB, was sucked out using Ureteral catheterunder vision that can be placed by side of telescope (unlike rigid suction that requires removal of telescope and before or after removal of FB).
FB was using optical forceps. Nature and location of FB, (whether UL or BL), number of attempts for grasping and removal of FB, operative time, intra and post-operative complications and post-operative stay in hospital were documented based on medical records and operative videos.
Results
Forty two patients 12 infants, 30 were more than 1 year; 26 were males and 16 females (male/female ratio being 1.62:1) were included in the study. Duration of FB in respiratory tract ranged from 6 hours to 8 months. 39 patients had unilateral and 3 had bilateral FB. N = 32 (76.19%) patients had organic FB, like peanut (most commonly raw and roasted were observed), betel nut piece, almond seed, green gram, tamarind seed, fruit seeds like custard apple were found. N = 10 (23.81%) patients had non-vegetative FB like stone, screw, safety pin, dental needle, nail, plastic paper, plastic whistle.
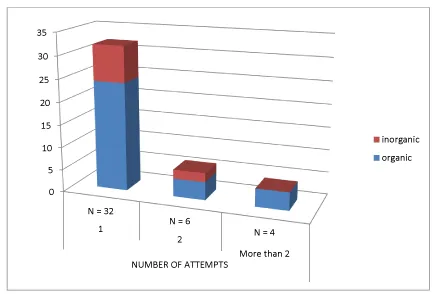
Number of attempts required to remove FB were evaluated based on operative video. 32 patients required 1 attempt, 6 patients required 2 attempts, and 4 patients needed more than 2 attempts (Graphs 1,2).
Operative time ranged from 15 min to 75min with mean of 32.6 minutes for organic FB and 18.2 minutes for inorganic FB (Table 1).
Out of 42 patients, 4 patients had complications that included bleed due to mucosal injury, 4 patients required post-operative intubation and ventilator support for few hours.Post-op stay lasted from 1 to 4 days with no mortality or failure of procedure.
Discussion
FBA is commonly observed in children. It is more common in boys, less than 3 years of age [4]. The increased risk is in part due to the lack of molar teveth and the exploration by mouth [2,5,6]. Our study revealed, 61.9 % of patients were male most of them were below 3 year. Other extant studies have indicated similar prevalence in boys [6,7].
Diagnosis was made using x-ray chest, and fluoroscopic evaluation. Computed tomography was required only in 14.29 % of patients along with detailed history and clinical evaluation. CT thorax with virtual bronchoscopy is a more useful method in organic FBA [8-10].
Nature of FB was organic in 76.19% of patients. Most common FB present was peanut and remaining patients had inorganic FB like metal, plastic or rarely stone. Boufersaoui, et al. (2013) have found aspirated bodies were organic in 66.7% patients, most of which included peanuts; sunflower seeds, beans and ears of wheat are considered as most dangerous. In other cases, FB were metallic or plastic such as pen caps, and recently, scarf pins [2,11-13].
In our study, mean operative time was more for organic FB than for inorganic FB similar to previous studies in literature. Boufersaoui, et al. (2013) have observed that endoscopic removal of FBs was successful in 97% of the cases and was completed (extracted?) in first attempt in 86% cases. In rare cases, (11%), it took until 3 attempts to remove all the residual fragments. In our study, endoscopic removal by rigid bronchoscopy was successful and completed in 100% cases with first successful attempt in 76.19% of patients, and only 9.52% of patients required more than two attempts. The intraoperative complications related to the endoscopic procedure were found in 9.52% of the patients in the form of bleeding due to mucosal injury. Only 4.76% of patients required ventilator support without any mortality [11,15-19].
In the initial two years from 2013 to 2015 of learning curve, we have used rigid metallic suction cannula (Karl Storz), in which blind suctioning required more operative time. Hence we developed indigenous flexible suction catheter using ureteric stent. It is easily available, disposable and economical, especially in rural India (Table 2). To the best of the authors’ knowledge, no prior study has included any reference or suggested this kind of technique.
Conclusion
Use of Ureteral catheter for under vision suctioning in rigid bronchoscopy in children is quite feasible and effective technique. The main advantages of this technique are simplicity, short operative time, less traumatic, good vision, with minimal complications.
- Divisi D, Di Tommaso S, Garramone M, Di Francescantonio W, Crisci RM, et al. (2007) Foreign bodies aspirated in children: role of bronchoscopy. Thorac Car diovasc Surg 55: 249‐252. Link: https://bit.ly/2ByRjtj
- Boufersaoui A, Smati L, Benhalla KN, Boukari R, Smail S, et al. (2013) Foreign body aspiration in children: experience from 2624 patients. Int J Pediatr Otorhinolaryngol 77: 1683-1688. Link: https://bit.ly/2BxI2lg
- Soysal O, Kuzucu A, Ulutas H (2006) Otolaryngol Tracheobronchial foreign body aspiration: a continuing challenge. Otolaryngol Head Neck Surg 135: 223-226. Link: https://bit.ly/3jG88nn
- Mnejja M, Chakroun A, Bougacha L, Smaoui L, Ben Salah M, et al. (2012) Bronchoscopy for foreign body inhalation in the pediatric population: lessons learned from 223 cases. Arch Pediatr 19: 670‐674. Link: https://bit.ly/32Yz23S
- Hebbazi A, Afif H, El Khattabi W, Aichane A, Bouayad Z (2010) Scarf pin: a new intrabronchial foreign body. Rev Mal Respir 27: 724‐728. Link: https://bit.ly/303bPMg
- Skoulakis CE, Doxas PG, Papadakis CE, et al. (2000) Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int J Pediatr Otorhinolaryngol 53: 143‐148.
- Saki N, Nikakhlagh S, Rahim F, Abshirini H (2009) Foreign body aspirations in infancy: a 20-year experience. Int J Med Sci 6: 322‐328. Link: https://bit.ly/3f45fJm
- McGuirt WF, Holmes KD, Feehs R, Browne JD (1988) Tracheobronchial foreign bodies. Laryngoscope 98: 615‐618. Link: https://bit.ly/39us201
- Hajnal D, Kovács T (2018) Foreign Body Aspiration of the Lower Airways in Children - Diagnosis in Clinical Practice. Orv Hetil 159: 2162-2166. Link: https://bit.ly/302jJFD
- Sink JR, Kitsko DJ, Georg MW, Winger DG, Simons JP (2016) Predictors of Foreign Body Aspiration in Children. Otolaryngol Head Neck Surg 155: 501‐507. Link: https://bit.ly/3hzwVaI
- Mohammad M, Saleem M, Mahseeri M, Alabdallat I, Alomari A, et al. (2017) Foreign body aspiration in children: A study of children who lived or died following aspiration. Int J Pediatr Otorhinolaryngol 98: 29‐31. Link: https://bit.ly/2X1fwA1
- Mnejja M, Chakroun A, Bougacha L, Smaoui L, Ben Salah M, et al. (2012) Bronchoscopie pour inhalation de corps étrangers chez l'enfant : à propos de 223cas [Bronchoscopy for foreign body inhalation in the pediatric population: lessons learned from 223 cases. Arch Pediatr 19: 670‐674. Link: https://bit.ly/3g6Le6k
- Oncel M, Sadi Sunam G, Ceran S (2012) Tracheobronchial Aspiration of Foreign Bodies and Rigid Bronchoscopy in Children Pediatr Int 54: 532-535. Link: https://bit.ly/3hIjQfB
- Albirmawy OA, Elsheikh MN (2011) Foreign body aspiration, a continuously growingchallenge: Tanta University experience in Egypt, Auris Nasus Larynx 38: 88-94. Link: https://bit.ly/39tNhyS
- Midulla F, Guidi R, Barbato A, Capocaccia P, Forenza N, et al. (2005) Foreign body aspiration in children. Pediatr Int 47: 663‐668. Link: https://bit.ly/2BwNvZx
- Foltran F, Ballali S, Passali FM, Kern E, Morra B, et al. (2012) Foreign bodies in the airways: a meta-analysis of published papers. Int J Pediatr Otorhinolaryngol 76: S12‐S19. Link: https://bit.ly/3g5NXwV
- Susy Safe Working Group (2012) The Susy Safe project overview after the first four years of activity. Int J Pediatr Otorhinolaryngol 76: S3‐S11. Link: https://bit.ly/2D7eHP1
- Kim IA, Shapiro N, Bhattacharyya N (2014) The national cost burden of bronchial foreign body aspiration in children. Laryngoscope 125: 1221-1224. Link: https://bit.ly/2Ee5NzJ
- Skoulakis CE, Doxas PG, Papadakis CE, Proimos E, Christodoulou P, et al. (2000) Bronchoscopy for foreign body removal in children. A review and analysis of 210 cases. Int J Pediatr Otorhinolaryngol 53: 143‐148. Link: https://bit.ly/2BCeanY
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.





 Save to Mendeley
Save to Mendeley
