Archives of Otolaryngology and Rhinology
Second localization of a lymphoma affecting the nasopharynx
MS Diouf*, M Ndiaye, F Fall, A Thiam, A Diop and R Deguenonvo
Cite this as
Diouf MS, Ndiaye M, Fall F, Thiam A, Diop A, et al. (2023) Second localization of a lymphoma affecting the nasopharynx. Arch Otolaryngol Rhinol 9(2): 003-005. DOI: 10.17352/2455-1759.000150Copyright
© 2023 Diouf MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.Non-Hodgkin lymphomas are lymphoid malignant neoplasms with diverse biological and clinical behavior. They rarely affect the nasopharynx. Most patients respond well to chemotherapy, which may be combined with radiotherapy but relapses are frequent.
We report the case of a 52-year-old female patient first treated for abdominal B lymphoma which recurred 13 years later in the nasopharynx after a complete response to initial treatment.
The patient complained of rhinolalia and bilateral purulent rhinorrhea. Chemotherapy controlled the lesion.
Thus we must consider a second nasopharyngeal location of NHML in cases of nasopharyngeal signs with associated cervical lymph nodes.
Introduction
Lymphoma of the cavum accounts for 4% of all cancers of the nasopharynx [1]. It comprises two main histological entities: Hodgkin lymphoma and Non-Hodgkin Lymphoma (NHL). NHLs tend to be extranodal, and their locations fall into two distinct categories: the lymphoid organs of Waldeyer's ring, and extra-nodal extralymphoid locations. Non-Hodgkin's malignant lymphomas (NHML) are the most common hematological malignancies [2], but their nasopharyngeal localization is rare. NHML is more frequent in the ENT sphere than Hodgkin lymphoma [3].
We report the case of a patient with recurrent abdominal non-Hodgkin's malignant lymphoma secondarily involving the rhinopharynx.
Clinical case
This is a 52-year-old female patient with a 17-year history of diffuse large-cell B lymphoma in the abdominal lymph nodes. She was treated with chemotherapy (8 courses, CHOP protocol) followed by radiotherapy with a complete response.
Four years ago, the patient complained of rhinolalia and bilateral purulent rhinorrhea. We noted the absence of a blocked nose, rhinorrhea, and epistaxis. The patient did not mention hearing loss or fever.
The examination found bilateral and asymmetrical cervical and axillary lymph nodes measuring 3 cm long.
Flexible nasoendoscope examination revealed an ulcerative and bleeding mass filling the entire nasopharynx.
A panendoscopy was performed under general anesthesia with orotracheal intubation. It revealed the same mass, which was ulcerative and budding, occupying the entire rhinopharynx. A biopsy was performed occasionally.
The blood test had not been requested. Histological examination concluded that it was a recurrence of malignant non-Hodgkin's lymphoma.
Immunohistochemistry revealed a diffuse B lymphoma rich in T lymphocytes (CD20+, CD3+, and 79a+).
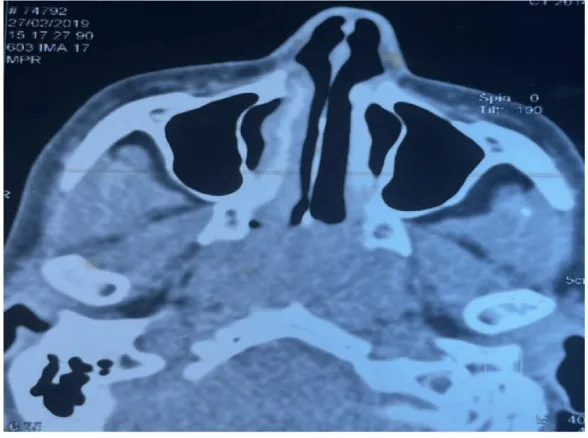
The CT scan revealed the filling of the entire cavum by a tissue process (Figure 1), as well as bilateral axillary and supra-clavicular adenopathies.
A thoracic-abdominal-pelvic CT scan revealed no secondary localization.
The patient received further courses of chemotherapy: a COP cytoreduction course followed by 6 courses of R-CHOP-Bleomycin with 4 courses of intrathecal chemotherapy.
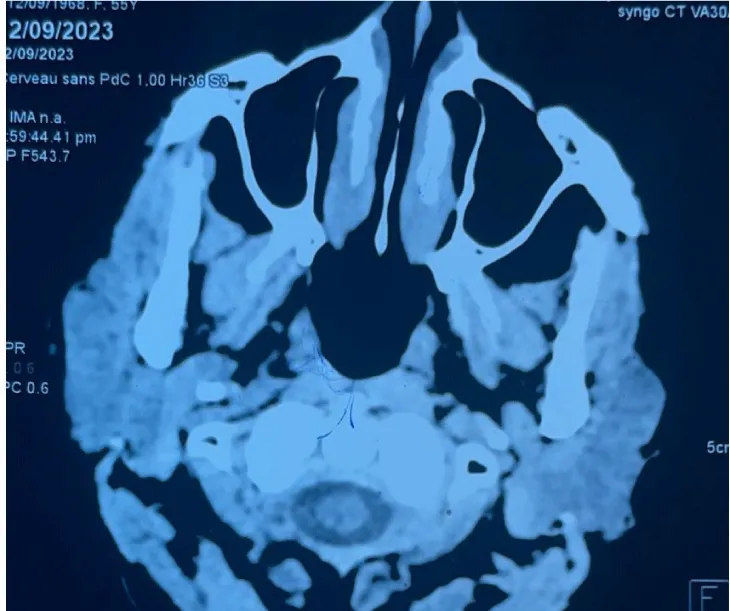
Control CT was normal 6 months after chemotherapy (Figure 2). A follow-up panendoscopy revealed a budding mass in the right Rosenmüller fossa and the roof of the cavum. Pathological examination revealed the absence of lymphomatous proliferation.
The patient has been in remission for 2 years, with a normal follow-up CT scan dating back 2 months.
Discussion
NHML can occur at any age, but more often between the fifth and sixth decades, as was the case in our patient. Nevertheless, it is most frequently seen in males (sex ratio 3.6) [4].
The clinical signs most frequently found in cases of nasopharyngeal involvement are nasal obstruction, hearing impairment, and cervical lymph nodes. Diagnosis is usually made early (80% in stages I and II) [5]. Adenopathies are usually found in half of all cases and are firm, mobile, and not painful. General signs are found in 20% of cases, and cranial nerve involvement is extremely rare [3]. In contrast, aggressive DLBCL and Burkitt's lymphomas have noisy symptoms and may require intensive care [3].
Diagnosis of nasopharyngeal NHML is based on an endoscopic biopsy of the rhinopharynx. An immunohistochemical study is essential to confirm the lymphomatous nature of the tumour and to reveal the phenotype of the tumour cells (expression of CD20 for the B phenotype, and CD56 and CD45RO for the T phenotype). The B phenotype predominates in LMNH of the cavum (60%).
Radiology is an essential part of the extension work-up for these tumours. The superiority of MRI of the cavum over CT has been established, particularly for the exploration of the deep spaces of the face. However, CT still has its place when it comes to studying the cortical bone at the base of the skull. Exploration of the neck as far as the supra-clavicular recesses is recommended in search of extension [2].
The prognosis of rhinopharyngeal NHML depends on histological grade, initial stage of disease, international prognostic index, and response to initial treatment [3]. In all cases, lymphomas are "chemosensitive" tumours, and treatment is always administered with curative intent, even in the event of relapse, and the prognosis remains favourable [1].
Our patient received chemotherapy according to the COP protocol followed by R-CHOP, as is the case for most NHML patients in low-income countries where access to Rituximab is still limited [6]. As NHML of the nasopharynx is rare, there is as yet no standardized treatment. The therapeutic management of rhinopharyngeal lymphoma follows the same principles as for other types of lymphoma. Treatment is based on chemotherapy alone or combined with radiotherapy, as decided at a multidisciplinary consultation meeting [1,2].
For localized lymphomas without risk factors, treatment combines chemotherapy (3 courses of CHOP) with radiotherapy, with good results in terms of both overall survival and relapse rate. For lymphomas with unfavorable prognostic factors, chemotherapy is intensified. Several protocols are available: ACVBP (Doxorubicin, Cyclophosphamide, Vindesine, Bleomycin, and Prednisone), CHOEP (CHOP and Etoposide), mega-CHOEP, or others. In patients aged over 70, the frail terrain calls for less toxic chemotherapy. Rituximab has been shown to be effective in the event of relapse [3].
As for radiotherapy, target volumes include Waldeyer's area and bilateral cervical lymph nodes, at a dose of 45 to 55Gy with conventional spreading and fractionation. It should be conformal in order to minimize damage to neighboring organs [3,7]. Late toxicities are dominated by xerostomia, trismus, skin fibrosis, auditory toxicity, and to a lesser degree, neurocognitive deficit. Other, much rarer complications can be lethal (carotid rupture, particularly in re-irradiation situations) [7].
We deduce from this presentation that the nasopharynx is a second localization site for abdominal NHML. Therefore, monitoring of the nasopharynx should be considered during check-up appointments.
Conclusion
NHML is a tumor that rarely affects the rhinopharynx. It responds effectively to chemotherapy, which may be combined with radiotherapy. Our case illustrates the possibility of nasopharyngeal involvement in non-head and neck lymphomas.
Ethics approval and consent to participate
The patient has given consent.
- Andriambelo RH, Randrianandraina MP, Refeno V. Oculomotor paralysis revealing a rhinopharyngeal lymphoma. Jaccr Africa. 2019; 3(4): 406-412.
- Ouraini S, Nakkabi I, Benariba F. Lymphome malin non hodgkinien du cavum: protocoles thérapeutiques et facteurs pronostiques [Non-Hodgkin lymphoma of the cavum: prognostic factors and therapeutic protocols]. Pan Afr Med J. 2015 Oct 16;22:153. French. doi: 10.11604/pamj.2015.22.153.7916. PMID: 26889334; PMCID: PMC4742015.
- Ouraini S, Nakkabi I, Benariba F. Lymphome malin non hodgkinien du cavum: protocoles thérapeutiques et facteurs pronostiques [Non-Hodgkin lymphoma of the cavum: prognostic factors and therapeutic protocols]. Pan Afr Med J. 2015 Oct 16;22:153. French. doi: 10.11604/pamj.2015.22.153.7916. PMID: 26889334; PMCID: PMC4742015.
- Jardel P, Thariat J, Blanchard P, Elloumi F, Toumi N, Bensadoun RJ. [Nasopharyngeal cancers, an overview]. Bull Cancer. 2014;101(5):445‑54.
- Tebra S, Mahjoubi K, Chaouach K, Laatiri A, Bouaouina N. À propos de quatre cas de lymphome malin non hodgkinien primitif du cavum [Non-Hodgkin lymphoma of the nasopharynx: a report of four cases]. Cancer Radiother. 2011 Jul;15(4):338-41. French. doi: 10.1016/j.canrad.2011.02.005. Epub 2011 Jun 12. PMID: 21664166.
- Zhou HY, Gao F, Bu B, Fu Z, Sun XJ, Huang CS, Zhou DG, Zhang S, Xiao J. Primary bone lymphoma: A case report and review of the literature. Oncol Lett. 2014 Oct;8(4):1551-1556. doi: 10.3892/ol.2014.2327. Epub 2014 Jul 9. PMID: 25202366; PMCID: PMC4156201.
- Thompson LD. Diffuse large B-cell lymphoma of the nasopharynx. Ear Nose Throat J. 2012 May;91(5):192, 194. doi: 10.1177/014556131209100506. PMID: 22614552.
Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.


 Save to Mendeley
Save to Mendeley
