Archives of Otolaryngology and Rhinology
Pathophysiologic Perspectives on Muscle Tension Dysphonia
James P Dworkin-Valenti*, Robert J Stachler, Noah Stern and Esmael H Amjad
Cite this as
Dworkin-Valenti JP, Stachler RJ, Stern N, Amjad EH (2018) Pathophysiologic Perspectives on Muscle Tension Dysphonia. Arch Otolaryngol Rhinol 4(1): 001-010. DOI: 10.17352/2455-1759.000065It is difficult to quantify the incidence of hyperfunctional muscle tension dysphonia (H-MTD). Although voice disorders in general have been noted to affect approximately 10% of the population in the United States, up to 40% of patient visits to voice specialists are for symptoms of H-MTD. Clearly this condition is a very common vocal pathology, yet its differential diagnosis is not always straightforward. The primary purpose of this tutorial is to present a comprehensive literature review on this condition, with particular focus on alternative etiologic theories and differential diagnostic and treatment techniques. The secondary purpose of this tutorial is to increase awareness that this disorder is a complex condition with highly variable causes, features, and treatment requirements. As a consequence of recent advances in the field of neurolaryngology, and for completeness, the neurological substrates of voice and speech production are also discussed in this review. This information is included to evoke a theoretical conversation about possible patho-neurologic correlates in some patients with H-MTD; especially those who do not respond favorably to standard behavioral therapy strategies. Whereas only a brief discussion of treatment options is rendered in this paper, more detailed information on this topic will be covered in a forthcoming companion tutorial.
Introduction
It was more than 60 years ago that the concept of a physiologic linkage between the respiration, phonation, articulation, and resonation subsystems was proposed; that excess tension originating at any level of this unified speech production mechanism may result in referred hypertonicity and hyperfunction throughout this linear anatomical chain of musculoskeletal structures [1,2]. Since this seminal hypothesis, there have been countless investigations on the psychodynamic and pathophysiologic processes observed in individuals with hyperfunctional speech and voice disorders [3-17]. These inquiries have spawned numerous theoretical discussions about the most effective methods of differential diagnosis and treatment of these conditions.
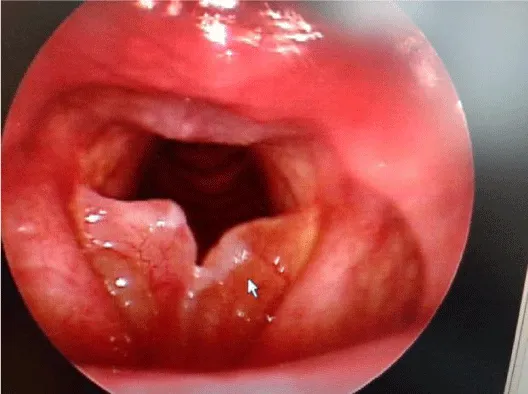
Individuals who exhibit forceful or excessive contractions of muscles that drive voice and speech production often struggle with a broad spectrum of associated abnormal signs and symptoms, including 1) harsh-shrill vocal quality, 2) limited pitch and volume control, 3) falsetto pitch breaks, 4) episodic arrests of phonation, 5) reduced maximum phonation time, 6) vocal fatigue, and 7) extrinsic laryngeal, intrinsic laryngeal, mandibular, and tongue musculature hypertension. When these abnormalities are not caused by obvious signs of phonation subsystem pathology or tissue trauma, the diagnosis of primary or non-phonotraumatic H-MTD is descriptively appropriate. Figures 1, 2, and 3 illustrate videostroboscopy findings from a healthy 16 year old female who initially presented to our voice laboratory with perceptual features of primary H-MTD that persisted for 18 months, including pressed voice and intermittent outbursts of shrill vocalizations. She denied any history of voice abuse behaviors. Note the normal appearing vocal folds at rest in Figure 1. Figure 2 demonstrates the onset of abnormal bilateral ventricular vocal fold activity during phonation effort (ie., plica ventricularis). Figure 3 shows full approximation of theses merging folds in concert with the aforementioned abnormal voice characteristics. This patient is a classic example of non-phonotraumatic H-MTD. She exhibits significant voice difficulty, owing to suppressive supraglottal hyperfunctional activity, in the presence of normal true vocal fold anatomy.
In contrast, organic or phonotraumatic H-MTD is the diagnosis ascribed to patients whose vocal hyperfunction results in the formation of benign unilateral or bilateral vocal fold lesions, such as nodules, discreet polyps, or Reinke’s edema [18-20]. Figures 4, 5, and 6 illustrate videostroboscopy findings from a 58 year old female who initially presented to our voice laboratory with harsh, shrill, husky vocal quality, with associated significant limitations in pitch and volume range and control. She exhibited hallmark Type-A personality characteristics, with associated aggressive voice behaviors in all social settings; she also struggled with chronic sleep apnea. Note that Figure 4 shows an advanced degree of bilateral Reinke’s edema, vocal fold erythema, and airway dimension compromise. These findings easily explain the chief presenting vocal and sleep related complaints, and they are consistent with the patient’s voice abuse history. Figure 5 demonstrates the medial merging forces of the ventricular vocal folds, as the patient attempts phonation during the examination. This combination of causally inter-related traumatic tissue pathology and pathophysiological hyperfunctional voice behaviors contributed to a vicious cycle of abnormal conditions and factors, which required immediate aggressive intervention, including phonosurgical management and voice therapy. Figure 6 illustrates the patient’s 3-month post-treatment result. Note the healthier appearance of the true vocal folds and the dramatically reduced activity of the ventricular vocal folds during this phonatory frame.
In some patients with either the non-phonotraumatic or phonotraumatic subtype of MTD, co-existing respiration and/or articulation subsystem musculature hyperfunction exacerbates the voice problem. It has been estimated that approximately 50 % of patients evaluated by otolaryngologists for voice complaints present with characteristics of hyperfunctional dysphonia [21].
The overall purpose of this paper is to render a comprehensive review of the scientific literature on H-MTD. Specific focus will be placed on 1) the essential neurological substrates of voice and speech production, 2) differential diagnosis of pathologic variants of this vocal pathology, and 3) treatment considerations. A forthcoming companion tutorial will provide detailed descriptions of alternative treatment strategies that have been reported for this condition over the past 5 decades, along with specific recommendations for future clinical research investigations.
Neurologic substrates of speech production
Our understanding of the complex neurological processes of voice production remains elementary to date. However, significant advancements are currently underway in neurodiagnostic testing, neurosurgical treatment techniques, and biomolecular and genetic engineering that should propel new and innovative methods of differential diagnosis and management of H-MTD. Improvements in our knowledge of open loop, closed loop, state, auditory, tactile, and proprioceptive feedback control models of speech production may help explain the variable characteristics of this vocal pathology and ensure the evolution of more efficient evaluation and treatment procedures. Specific test results that offer reliable explanations for the multi-varied voice difficulties exhibited by patients with this condition may lead to the development of type-specific management algorithms.
The end-organ
In all mammals, the larynx serves 3 vital functions: 1) promotes a patent airway for various respiratory demands, 2) primitively protects the airway during swallowing activities, and 3) works harmoniously with the breathing mechanism to drive both deliberate and autonomic vocalizations, which in humans may be converted into articulated speech. Although the first two functions can be temporarily modulated by voluntary efforts, for the most part they are regulated by involuntary processes mediated by brainstem reflexive pathways. The third function is more complicated in that successful execution of verbal speech is dependent upon complex cooperation, integration, and physiologic integrity of numerous muscles groups of the head, neck, thorax, and abdomen. These collectively help to form the 4 primary speech subsystems: respiration, phonation, articulation and resonation.
Neurolaryngology
In general, cooperative contractions of the above mentioned muscle groups are all initially driven by voluntary central nervous system motor pathways, via finite synaptic connections with various cranial and spinal nerves of the peripheral nervous system. Within this final common pathway of neuromuscular stimulation there are many reflex arcs that regulate most movements and contribute to the feedback circuitry between the periphery and the brain. In addition, and specific to the phonation subsystem, the endolarynx possesses a very rich supply of sensory nerve endings that are extremely important both for airway protection and regulation of voluntary respiratory events that occur during speech activities. The recurrent and superior laryngeal nerves, both branches of the Vagus nerve, are the prime conveyers of sensory information from the glottis and supraglottis, respectively. Their cell bodies are located within the nodose ganglion, the larger of the two sensory ganglia of the Vagus nerve. This bundle of neurons is located immediately below the jugular foramen. It contains both somatic and visceral sensory components, which project to the spinal trigeminal and solitary tracts of the brainstem, respectively. In addition to these primary sources of end organ sensation, the laryngeal mucosal lining, all intrinsic muscles and joints of the larynx, and walls of the trachea are invested with different types of mechanoreceptors that significantly mediate respiratory and vegetative reflexes via their interfaces with the aforementioned laryngeal nerves. It has been suggested that these reflex arc transmitters function as critical participants of an intrinsic laryngeal monitoring system by relaying sensory information to the lower brainstem about air pressure variations within the immediate subglottis and larynx during phonation. This receptor-myotatic reflex mechanism contributes to 1) position and movement adjustments of the cartilaginous framework of the larynx during speech and singing activities, and 2) inhibitory and facilitory regulation of variable tension levels of the vocal folds associated with such vocalizations. This neuroanatomic circuitry constitutes the so-called tonic servo-reflex system within the larynx [22-29].
Voluntary activation and operation of the laryngeal peripheral biofeedback system, largely depend upon descending motor stimuli from the corticobulbar tracts of both frontal lobes of the brain to the motor neuron pools of the Vagus nerve within the nucleus ambiguous of the medulla; synchronous corticospinal tact stimuli are concurrently transmitted to spinal nerves along the spinal cord so that cooperative breath support can accommodate all voice activities. Together these upper motor neuron tracts comprise the pyramidal system, and they are the primary stimulants of all voluntary voice and speech musculature contractions. Parallel sensory pathways, originating in the nerves and mechanoreceptors within the musculature, joints, and mucosa of the peripheral end organs, project to the brainstem, subcortical way-stations, and parietal lobes of the brain to complete the speech mechanism sensory-motor neuroanatomic loop.
Sensory-motor feedback
Although there is little debate about the existence of these neural pathways, neuroscientists and voice specialists are not certain that acts of voluntary phonation require ongoing monitoring or regulation by this servo system. Studies have clearly demonstrated that even in the absence of sensory feedback from the larynx subjects are usually able to maintain gross motor voice ability with minimal disturbances in pitch, volume, or vocal quality control [30-33]. These results support the hypothesis that normal voice production depends more on “open-loop” feedback operations than “closed loop” principles; the former process functioning independent of sensory information from the larynx or its central nervous system coordinates. The balancing effects of the auditory feedback system have been characterized as significant contributors to the preservation of near normal voice ability under laryngeal deafferentation conditions [34,35]. We would suggest that whereas sensory feedback may not normally be required to initiate and sustain voice, such continuous information from the end organ likely provides on-line input regarding the functional status of vocal fold vibrations and whether there is a need for corrective actions to achieve all target speech behaviors. Such sensory assurances or warnings may increase the overall physiologic efficiency of contextual speech production, even if such feedback only serves as an ancillary assistant when necessary. We further propose that prolonged disturbances in or dysregulation of this volitional-reflexive neuromuscular circuit within and between the various subsystems of the speech mechanism, regardless of the associated etiology, may be responsible for motor speech difficulties, including some variants of H-MTD. This hypothesis may be especially testable in individuals with this vocal pathology who have no history of psycho-emotional conflicts and for whom standard behavioral therapy paradigms are ineffectual. In support of this line of reasoning, several researchers have suggested, based on their clinical experiences and experimental investigations that the larynx can accomplish primary motor functions because of the indispensable feedback support it receives from its sensory and autonomic properties [36-38]. Additionally, there is an abundant data base on patients with irritable larynx syndrome, owing to depressed or heightened neurosensory thresholds or sensitivity. This clinical population frequently presents with one or more of the following disorders: Chronic cough, paradoxical vocal fold motion abnormalities, incessant throat clearing, laryngospasms, and H-MTD [39-41]. These conditions are often attributable to viral upper respiratory infections, laryngopharyngeal reflux events, chronic cigarette use or exposure, protracted use and misuse of steroidal inhalers, direct tissue trauma, and psychogenic factors. It has been suggested by these researchers that future treatment programs for this spectrum of disorders may need to target the laryngeal sensory-reflexive feedback system, at least for the subset of patients who are recalcitrant to behavioral therapies of one type or another.
Neurologic schema of voice and speech production
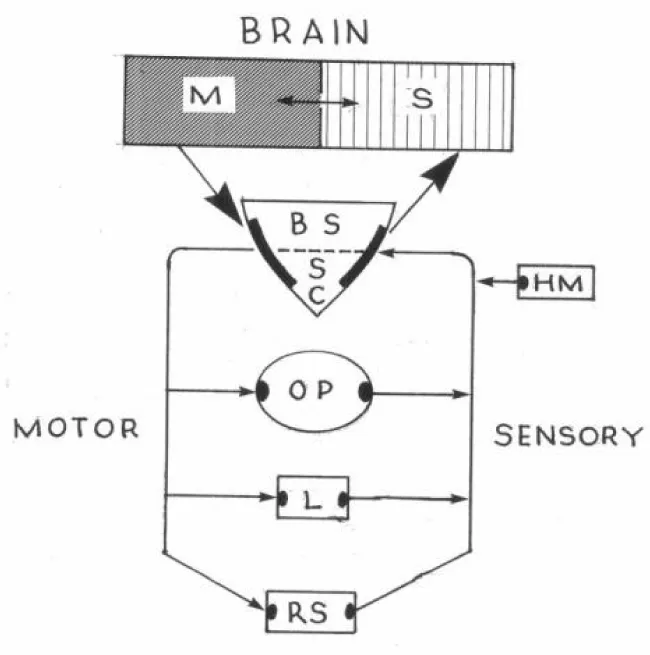
Figure 7 illustrates the proposed sensory-motor reflex monitoring loop of a normal speech mechanism. This diagram is meant to demonstrate, as simplistically as possible, the descending and ascending neuromuscular pathways within and between the various components of this musculoskeletal complex. Note the neuroanatomical hierarchy: Neural stimuli to initiate preplanned volitional speech behaviors originate in the motor cortex (M) of the brain and travel caudally and sequentially as elongated pyramidal tract fibers through the subcortex to the brainstem (BS), spinal cord (SC), oropharynx (OP), larynx (L), and respiratory subsystem (RS). Also note the reverse ascending sensory pathways from these same structures to the sensory cortex (S). It is important to consider that vital contributions to these loops of motor and sensory processing are made by components of the extrapyramidal system, including the thalamus, basal ganglia, and cerebellum. These subcortical structures establish complex pedunculated neural projections among themselves and the motor and sensory cortex. The acronym HM represents the role and importance of the hearing mechanism for continuous auditory feedback, as mentioned earlier. This multilayered and parallel circuit constitutes and completes the feedback loops and reflex monitoring system. When functioning normally these pathways work harmoniously to ensure smooth, synchronous, and appropriately forceful muscle contractions required for articulate and fluent speech. It could be argued that these sensory-motor neurologic circuits serve to check and balance all activities within and between system components, and, as noted above, they provide various forms of feedback regarding the need for corrective actions to ensure that specific speech targets are produced successfully.
H-MTD: differential etiologies, features, and testing
Alternative Causal Associations: The etiologies of H-MTD remains a topic of considerable debate. Clinical researchers have suggested that causal factors usually vary from patient to patient, but often include one or more of the following abnormal behavioral or functional conditions: 1) notable degrees of psycho-emotional stress and personality disorders, 2) compensatory forceful voice efforts that persist long after symptoms of an acute voice abuse event or upper respiratory infection have resolved, 3) laryngeal tissue erythema and edema secondary to the effects of laryngo-pharyngeal reflux, and 4) variable neuromotor and/or neurosensory abnormalities of the muscles, joints, and mucosa that comprise the aforementioned 4 speech subsystems [9,41]. We strongly propose that the first of these contributing factors is very frequently associated with the onset of the non-phonotraumatic (primary) variant of H-MTD. To support the plausibility of this hypothesis, we discovered several investigations on psychological and personality trait factors in patients with this diagnosis. In general, results revealed a measurable trend toward variably elevated levels of introversion, neurotism, depression, stress reactivity, and anxiety among this population [-9,42-45]. In concert with these findings, we have discovered that for many of our own patients with primary H-MTD, psychotherapy has played an indispensable role in their overall rehabilitation programs. In contrast, the extent to which any of the remaining 3 causal factors listed above may contribute to the development of H-MTD tends to be uniquely variable and unpredictable from patient to patient. As such, differential diagnosis and treatment of this disorder are inherently challenging tasks because of the broad spectrum of possible patient presentations. Theoretically, to ensure accurate diagnosis in each case, appraisal techniques should include comprehensive tests and measures for each of these 4 possible causal factors.
A condition labeled laryngeal tension-fatigue syndrome was described 15 years ago in more than 300 patients with chronic functional dysphonia due to vocal abuse and misuse [46,47]. Most of these subjects exhibited stroboscopic evidence of multiple vocal fold cover abnormalities, owing to hyperfunctional muscle tension voice behaviors, and biomechanical tissue pathologies secondary to associated phonotrauma. It is interesting to speculate whether or not these patients struggled with inherent bioenergetic weakness of the intrinsic laryngeal skeletal muscles, which in turn resulted in these pathophysiologic sequelae. Whether or not laryngeal EMG and speech aerodynamic testing would have shed additional light on this hypothesis is an interesting question, which deserves further investigation.
A recent review of intrinsic laryngeal skeletal muscle physiology suggested a possible causal relationship between H-MTD and phonation subsystem bioenergetic fatigue [48]. Proponents of this pathophysiologic association have hypothesized that as voice expression weakens under such conditions the individual employs compensatory hyperfunctional vocal behaviors to overcome the problem. If this activity persists, it then may become sustained through subconscious mechanisms, leading to cyclically habitual pressed voice characteristics. The unfortunate outcome of these bioenergetic events involving the laryngeal musculoskeletal system is an exacerbation of the emergent voice disorder, with deterioration of vocal quality, pitch and loudness control. These clinical researchers have suggested that voice remediation in such cases would theoretically benefit from specific fatigue resistance and mechanical stress reduction respiration, phonation, and articulation subsystem exercises.
Adding to the theoretical treatise on causal associations, researchers have recently employed functional MRI technology to study brain activity during phonation in individuals with H-MTD [49]. Preliminary results demonstrated that in comparison to a control group with normal voices, these subjects exhibited higher degrees of pre-central gyrus, inferior, middle and superior frontal gyri, lingual gyrus, insula, cerebellum, midbrain, and brainstem activities. Additionally, comparatively lower activation patterns were noted in the cingular gyrus, temporal gyrus, and inferior parietal lobe regions in the H-MTD experimental group. Discussions regarding the possible neurophysiological mechanism overlying laryngeal hyperfunction and tension voice disorder were offered for differential diagnostic and treatment considerations.
Other clinical researchers have corroborated the aforementioned low level temporal lobe FMRI results with preliminary evidence of abnormally depressed degrees of auditory feedback and motor speech adaptation responses in individuals with H-MTD [50]. Based on these experimental findings these investigators hypothesized that in some patients who struggle with this vocal pathology there may be a neuropathologic explanation, owing to disruptions in auditory-motor integration and feedback normally required to regulate fluent contextual speech.
Because of the characteristic voice profiles of many individuals with H-MTD, researchers have studied the speech aerodynamic behaviors in this clinical population. They have hypothesized that dysregulation of the respiratory subsystem during voice production may be causally related to their notable strained and pressed voice quality features [18,51]. Examination of subglottic pressure, glottal resistance, and transglottal airflow rate values revealed variable levels on these parameters, but mostly within normal limits. These investigators remained puzzled regarding why many such patients exhibit observable choppy breathing patterns during conversational speech in the presence of speech aerodynamic physiologic integrity. They suggested that future investigations regarding why and how abnormal respiratory patterns develop in the first place should be conducted. As previously recommended, we would also suggest that the most valuable answers to these questions will be derived from the study designed to evaluate patients with different degrees and potentially variable etiologies of H-MTD.
More recently, cortical excitability differences between individuals with H-MTD and those with focal laryngeal dystonia (ie., adductor spasmodic dysphonia) were investigated using transcranial magnetic stimulation [50]. This study was undertaken because of the striking perceptual similarities between these two vocal pathologies. Results of such experiments demonstrated that those with spasmodic voices exhibited significantly shorter cortical silent periods involving the orofacial musculature than those with H-MTD. Whereas these findings strongly supported long-standing implications of dysfunctional extrapyramidal system pathways overlying spasmodic dysphonia [52], the results did not unequivocally reveal central or peripheral nervous system correlates of H-MTD. Consequently, the investigators of this interesting research project were unable to recommend use of this technology in the differential diagnosis of this latter disorder. For completeness, they did not classify or segregate the subjects in this study group according to their severity and/or possible variant subtype (eg., psychogenic Vs. neurogenic) prior to testing. Had the study design considered this hypothetical sub-classification of patients with H-MTD, perhaps the results might have been conceptually and diagnostically more intriguing and beneficial.
As a new and interesting dimension of inquiry, researchers in the field of neuropsychology have recently proposed that H-MTD in general ought to be considered as a new phenotype characteristic in some children with attention deficit hyperactivity disorder; particularly the phonotraumatic variant, because of the high incidence of vocal fold nodules in this population [53,54]). This multi-factorial neurobehavioral childhood disorder affects as many as 10% of all school-age children. It has been defined as a behavioral disorder of self-regulation, causally associated with dysfunction of the frontal-subcortical system and dysregulation of both dopamine and noradrenaline neurotransmission [55]. Along this line of reasoning, we suggest that for certain subsets of patients with H-MTD there may be an important role for comprehensive psychological and neurological evaluations in their diagnostic battery. We also suspect that emerging advancements in our understanding of the neurology of voice production will eventually lay the groundwork for more inclusive subspecialty laboratory and clinical consultations for most patients with this multi-factorial vocal pathology.
For academic discussion and eventual clinical remedies, we offer the suggestion that patients with H-MTD who are recalcitrant to behavioral intervention techniques represent a more complex subset of this clinical population; individuals whose pathophysiologic muscle tension vocal behaviors may prove to be more organic in origin than functional. That is to say, perhaps for these individuals our diagnostic lenses must be refocused to sharpen the search beyond psychogenetic factors in favor of other explanations, such as 1) occult end organ pathology (eg., vocal fold paresis or sulcus formation), and/or 2) laryngeal sensory-motor abnormalities. These conditions represent very interesting pathogenetic factors that may be causally related to the onset of H-MTD in some cases. Opportunities for experimental research in these areas of inquiry are boundless, especially with respect to treatments that may be oriented toward these possible etiologies.
Characteristics and appraisal
To date, accurate identification and classification of H-MTD are largely dependent upon the collective results of the clinical examination and laryngeal endoscopy; there are no standard objective tests or tools that must be used for the unequivocal diagnosis of this disorder. Quite often, the differential diagnosis is reached by exclusion. However, because the associated auditory-perceptual voice characteristics often mimic the features of other voice disorders, such as previously mentioned adductor spasmodic dysphonia or compensatory strained phonation caused by laryngeal end organ pathology, accurate diagnosis can be rather challenging; especially for the inexperienced clinician. Very valuable keys to the differential diagnosis of H-MTD are discovered from the results of the detailed case history. This is particularly true when palpable signs of neck and jaw hypertension are accompanied by variable complaints of high stress, anxiety, general malaise, odynophagia, globus sensation, muscle strain, and odynophonia [56-58]. Use of validated questionnaires to measure a patient’s self-impressions of voice production difficulties have been shown to reinforce the presumed diagnosis of H-MTD. These same clinical instruments have also been used constructively for ambulatory voice monitoring and to measure qualitatively perceived levels of voice improvement following treatment [59-61].
When examining an individual with suspected H-MTD, otolaryngologists and speech pathologists often rely on empirical clinical experiences and examination techniques that they routinely employ with any patient who presents with dysphonia. In general, they are challenged in two very important ways when preparing to evaluate the patient: 1) they must possess a fine auditory-perceptual filter for the differential identification of specific vocal quality, pitch and volume abnormalities that are pathognomonic of H-MTD, and 2) they must administer a reliable assortment of tests and procedures that may validate their perceptual impressions and distinguish all possible causes of the disorder. Regardless of the tests administered, the principle aims of the examination are to establish the differential diagnosis and a treatment plan that takes into consideration the suspected etiologic factors. With these objectives in mind, most voice specialists employ a testing format that includes a) various speaking tasks for auditory-perceptual voice appraisal, such as extemporaneous conversation, reading of a familiar passage, vowel prolongation, and singing, b) neck and laryngeal palpation to detect abnormal levels of muscular tension at rest and during speaking tasks, and c) laryngeal videostroboscopy to analyze the anatomical and physiological status of the vocal folds and surrounding soft tissue boundaries. In non-phonotraumatic H-MTD no specific laryngeal mucosal abnormalities will be observed during endoscopy. But, some patients may exhibit compensatory hyperkinetic false vocal fold (ie., plica ventricularis) and true vocal fold behaviors to achieve glottal closure; intermittent hard glottal attacks and anterior-posterior supraglottic contractions or squeezing commonly co-exist. Those who practice in academic settings have reported that various voice laboratory procedures, such as quantitative acoustic analyses, speech aerodynamic testing, laryngeal EMG, and laryngeal sensory measurements, may augment the auditory-perceptual and laryngeal endoscopic examination results [18,51,62,-64]. Recently, voice scientists have demonstrated that a small sample of women with H-MTD exhibited abnormally low sound pressure levels during glottal aerodynamic measurements. These findings led the researchers to conclude that during such testing this vocal hyperfunction subset of patients employed inefficient respiratory-phonatory mechanics, which decreased the collision forces of the vocal folds and paradoxically protected them from the development of mucosal lesions. If these preliminary results can be replicated with a broader demographic of patients with this disorder, another measurement tool can be included with confidence in the arsenal of testing, with the potential to influence approaches to treatment.
Several researchers have proposed the diagnostic importance of objective measures of hyoid bone and larynx motion during hyperfunctional voice behaviors [4,65]. Preliminary results of such investigations have revealed that individuals with H-MTD substantially and consistently speak with abnormally raised larynges in comparison to normal resting positions. This posturing pattern was construed to represent underlying hyperfunctioning of the extrinsic laryngeal musculature during pressed or strained voice production. To facilitate more elaborate analyses of hyolaryngeal muscle activation patterns in this clinical population these clinical investigators recommended further study using lateral cephalograms, video-fluoroscopic imaging, and laryngeal EMG recordings during various phonation tasks both during and following commonly used laryngeal massage and voice manipulation therapeutic techniques. In concert with such recommendations several researchers investigated extrinsic laryngeal muscle tension levels in individuals with H-MTD by studying surface EMG signals from supra and infrahyoid muscles [56]. Results of these studies did not demonstrate consistently abnormal EMG patterns during various speaking tasks in this clinical population. Use of EMG as a reliable diagnostic tool was not supported by these findings.
Treatment considerations
For discussion purposes, let us assume that there are acute and chronic varieties of H-MTD. That is to say, a) some patients who present with a self-limiting form of this disorder, owing to manifestations of an acute condition that ultimately resolves on its own without formal intervention, b) some patients whose acute dysphonia lingers well beyond resolution of the causal event and who seek medical treatment as a result, and c) some patients who struggle with intermittently or persistently chronic voice symptoms, caused by any number of different conditions as discussed earlier in this tutorial, for whom formal treatment appears necessary for the reacquisition of normal voice or to learn better compensatory voice behaviors. What’s more, it is not inconceivable that treatment requirements might materially differ between and within these latter two patient subgroups, based on the type-specific speech subsystem signs and symptoms and underlying causal associations in each case. Despite these well-established clinical caveats, behavioral voice exercises and circumlaryngeal massage continue to be the mainstay of treatment for the vast majority of individuals with H-MTD [66-70]. Perhaps this common routine may be why therapists and otolaryngologists alike are often frustrated by the fact that some patients respond quickly and dramatically to such treatments, but others experience little or no voice improvement, even after numerous therapy sessions. Within the last decade, clinical researchers have discussed the need to develop more effective and targeted treatment alternatives for those patients with H-MTD who do not respond to standard behavioral therapeutic strategies. That is, to construct for each case an individualized training paradigm that is consistent with the unique etiology and combination of speech subsystem abnormalities detected during the diagnostic evaluation.
In general, all speech rehabilitation programs operate on the fundamental goal of restoring verbal communication abilities to the original state prior to the onset of the problem. Voice skill acquisition through formal treatment of H-MTD may depend upon the extent to which the motor learning mechanisms are impaired in any given patient. This factor may only be gleaned during a comprehensive differential diagnostic examination battery, as has been discussed earlier in this tutorial; cursory appraisal techniques may yield insufficient information regarding the best course of management. As is true for many different clinical populations with speech disorders, canned therapy programs do not always result in the best treatment outcomes; even those designed on theoretically sound principles fail to help all patients. This observation is common among clinicians from all backgrounds and levels of experience; and astute practitioners quickly identify when it is necessary to introduce novel or perhaps experimental approaches to management. Within the realm of such reasoning, clinical researchers must design studies that strategically compare the efficacy of alternative treatments for H-MTD to determine if certain techniques are better than others for any given patient and why. Data from such investigations may produce varietal training algorithms for this multifactorial vocal pathology.
In addition to, or in lieu of, common voice exercises, some patients may be more responsive to one of more of the following experimental approaches to management: 1) sensory deafferentation of the immediate subglottis and endolarynx, 2) intrinsic auditory and visual feedback via acoustic and speech aerodynamic computer displays, 3) voice augmentation via laryngeal EMG and accelerometer biofeedback, 4) circumoral and circumlaryngeal neurofacilitation or neuroinhibition via reflex motor control stimulation techniques (eg., icing, warming, vibrotactile stimulation, counterbalancing resistance exercises, tonal reduction via stretching maneuvers, tendon pressure, and tendon tapping), to suppress aberrant muscle patterns and excite normal adaptations, and 5) laryngeal sensori-motor integration therapy [32,71-77]. We propose that any of these treatments, either alone or in combination with one another, may promote several important synergistic physiologic benefits, including 1) rebalancing central and peripheral neuromotor and neurosensory processes necessary to support relaxed and continuous vocalization efforts, 2) increasing kinesthetic and proprioceptive awareness of muscle tension levels during coordinated speech activities, 3) breaking the habitual cycle of hyperfunctional laryngeal and/or orofacial muscle behaviors, 4) jump-starting or re-setting integrative and controlled speech mechanism musculature contractions via manipulative muscle tone and strength exercises.
The foundation for these interventions and proposed mechanisms of action is constructed from an abundance of evidenced-based material within the motor speech therapy, physical therapy, occupational therapy, psychotherapy, and neurorehabilitation literature [78]. In general, all of these treatments are essentially designed to stimulate or inhibit the sensory, motor, and autonomic central and peripheral neural pathways and end organs that normally control and regulate voice and speech production. In our forthcoming companion tutorial, these approaches to management will be discussed in detail and they will augment our coverage of the most commonly employed behavioral voice therapy techniques for H-MTD.
Conclusions
The primary objective of this tutorial was to produce a comprehensive overview of the world literature on hyperfunctional voice disorders. To facilitate a deeper understanding of the multifactorial pathophysiology of these conditions, we included a brief review of the important neurophysiologic correlates of normal speech and voice production. This information was included to reinforce our understanding of the complex volitional and reflexive neuromotor and neurosensory processes that are normally required to induce phonation and regulate smooth vocal transitions during conversational speech. Within this context of neurolaryngology, the condition classified as non-phonotraumatic H-MTD was reviewed in detail. We demonstrated that whereas the etiology frequently varies from patient to patient, most patients with this suspected clinical diagnosis present with predominantly pressed or strained vocal characteristics that are often accompanied by choppy breathing patterns, episodic arrests of phonation, and vocal fatigue. We also highlighted the causal relationship between psychological stress and this diagnosis in many individuals.We cautioned that failure to recognize this well-documented fact may result in faulty or incomplete diagnostic testing, inaccurate diagnoses, and poor treatment outcomes. Focus was also placed on the importance of identifying many other possible causal associations, including laryngopharyngeal reflux, underlying laryngeal sensory-motor abnormalities, and occult end organ pathologies (eg., vocal fold paresis or sulcus formation), to ensure comprehensive knowledge of all contributing factors and the development of etiology-based treatment programs.
Testing strategies, including various speaking tasks for auditory-perceptual voice appraisal, neck and laryngeal palpation, and laryngeal videostroboscopy, were briefly described as essential techniques for differential diagnosis of this condition. The potential adjunctive diagnostic value of quantitative acoustic analyses and speech aerodynamic testing was also discussed. Although we reinforced the fact that behavioral voice therapy continues to be a mainstay of treatment for the vast majority of patients with H-MTD, we also cautioned that alternative approaches to management may be necessary for those patients who are recalcitrant to traditional treatments. Theoretical discussions were rendered relative to why this latter subset of patients may not always respond to standard therapeutic measures. Finally, we suggested that future research directions will be addressed in greater detail in a forthcoming companion tutorial on type-specific treatments for this multi-varied vocal pathology.
- Froeschels E (1952) Chewing method as therapy. Arch Otolaryngol 56: 427-434. Link: https://goo.gl/voDCzD
- Weiss DA, Beebe HH (1950) The Chewing Approach in Speech and Voice Therapy. Basel-New York: S. Karger Publishers 1950. Link: https://goo.gl/EN2Dky
- Morrison MD, Rammage LA, Belisle GM, Pullan CB (1983) Nichol H. Muscular tension dysphonia. J Otolaryngol 12: 302-306. Link: https://goo.gl/7ZmtH9
- Van Houtte E, Van Lierde K. Claeys S (2011) Pathophysiology and treatment of muscle tension dysphonia: A Review of the Current Knowledge. J Voice 25: 202-207. Link: https://goo.gl/LaHGMM
- Oates J, Winworth A (2008) Current knowledge, controversies and future directions in hyperfunctional voice disorders. Int J Speech Lang Pathol 10: 267-277. Link: https://goo.gl/6CkUXu
- Altman KW, Atkinson C, Lazarus C (2005) Current and emerging concepts in muscle tension dysphonia: a 30-month review. J Voice 19: 261-267. Link: https://goo.gl/uDhzyi
- Angsuwarangse T, Morrison M (2002) Extrinsic laryngeal muscular tension in patients with voice disorders. J Voice 16; 333-343. Link: https://goo.gl/GhXMex
- Khoddami SM Ansari NN, Jalaie S (2015) Review on laryngeal palpation methods in muscle tension dysphonia: validity and reliability issues. J Voice 4: 459-468. Link: https://goo.gl/SZoF8r
- Roy N (2003) Functional dysphonia. Current Opinion in Otolaryng & Head Neck Surg 11: 144-148. Link: https://goo.gl/JR6KD1
- Leonard R, Kendall R (199) Differentiation of spasmodic and psychogenic dysphonias with phonoscopic evaluation. Laryngoscope 109: 295-300. Link: https://goo.gl/txjtf3
- Butcher P (1995) Psychological processes in psychogenic voice disorder. Eur J Dis Commun 30: 467-474. Link: https://goo.gl/iDvhrq
- Torabi H Khoddami SM, Ansari NN, Dabirmoghaddam P (2016) The vocal tract discomfort scale: validity and reliability of the Persian version in the assessment of patients with muscle tension dysphonia. J Voice 6: 711-716. Link: https://goo.gl/CA8u1S
- Colton RH, Casper JK (2006) Understanding Voice Problems: A Physiological Perspective for Diagnosis and Treatment (3rd ed.). Baltimore MD: Lippincott, Williams & Wilkins.v Link: https://goo.gl/zGoFxd
- Dromey C, Nissen SL, Roy N, Merrill RM (2008) Articulatory changes following treatment of muscle tension dysphonia: Preliminary acoustic evidence. J Speech Lang Hear Res 51: 196-208. Link: https://goo.gl/s1i1SX
- Hillman RE, Holmberg EB, Perkell JS, Walsh M, Vaughan C (1989) Objective assessment of vocal hyperfunction: An experimental framework and initial results. J Speech Hear Res 32: 373-392. Link: https://goo.gl/C5hKMs
- Roy N (2008) Assessment and treatment of musculoskeletal tension in hyperfunctional voice disorders. Internat J Speech-Lang Path 10: 195-209. Link: https://goo.gl/gjv76X
- Roy N, Nissen SL, Dromey C Saper S (2009) Articulatory changes in muscle tension dysphonia: Evidence of vowel space expansion following manual circumlaryngeal therapy. J Commun Dis 42: 124-135. Link: https://goo.gl/XaDFVd
- Espinoza VM, Zanartu M, Van Stan JH, Mehta DD, Hillman RE (2017) Glottal aerodynamic measures in women with phonotraumatic and nonphonotraumatic vocal hyperfunction. J Speech Lang Hear Res 60: 2159-2169. Link: https://goo.gl/FGwM1U
- Hillman RE, Holmberg EB, Perkell JS, Walsh M, Vaughan C (1990) Phonatory function associated with hyperfunctionally related vocal fold lesions. J Voice 4: 52-63. Link: https://goo.gl/KqcU1t
- Khoddami SM, Ansari NN, Izadi F, Moghadam ST (2013) The assessment methods of laryngeal muscle activity in muscle tension dysphonia: A review. The Scientific World J 10: 1155-1161. Link: https://goo.gl/HkW27c
- Bhattacharyya N (2014) The prevalence of voice problems among adults in the United States. Laryngoscope 124: 2359-2362. Link: https://goo.gl/novUVW
- Davis P, Nail B (1987) Quantitative analysis of laryngeal mechano-sensitivity in the cat and rabbit. J Physiol 388: 467-485. Link: https://goo.gl/wRewu8
- Kirchner J, Wyke B (1965) Afferent discharges from laryngeal articular mechanoreceptor. Nature 205: 86-87. Link: https://goo.gl/ZshmxV
- Mathew O, Sant'Ambrogio G, Fisher J, Sant'Ambrogio F (1983) Laryngeal pressure receptors. Respir-Physiol 54: 317-330. Link: https://goo.gl/k9EogQ
- Kirchner J, Suzuki M (1968) Laryngeal reflex and voice production. Ann NY Acad Sci 155: 98-109. Link: https://goo.gl/zety6K
- Suzuki M, Kirchner J (1969) Sensory fibers in the recurrent laryngeal nerve. Ann Otol Rhinol Laryngol 78: 1-30. Link: https://goo.gl/8wdS4n
- Sampson S, Eyzaguirre C (1964) Some functional characteristics of mechano-receptors in the larynx of the cat. J Neurophysiol 27: 464-480. Link: https://goo.gl/J3cLxg
- Abo-El-Enein M, Wyke B (1966) Laryngeal myotatic reflexes. Nature 209: 682-686. Link: https://goo.gl/P3Ncjb
- Cooper D, Lawson W (1992) Laryngeal sensory receptors. In: Blitzer A, Brin M, Sasaki C, Fahn S, Harris K, eds. Neurologic Disorders of the Larynx. New York, NY: Thieme 12-28. Link:
- Tanabe M, Kitajima K, Gould W (1975) Laryngeal phonatory reflex: the effect of anesthetization of the internal branch of the superior laryngeal nerve: acoustic aspects. Ann Otol Rhinol Laryngol 84: 206-213. Link: https://goo.gl/3j8RMH
- Sorenson D, Horii Y, Leonard S (1980) Effects of laryngeal topical anesthetic on voice fundamental frequency perturbation. J Speech Hear Res 23: 274-283. Link: https://goo.gl/UUwFBe
- Dworkin JP, Meleca RJ, Simpson ML, Garfield I (2000) Use of topical lidocaine in the treatment of muscles tension dysphonia. J Voice 14: 567-574. Link: https://goo.gl/QVh1gS
- Scott-Kelso JA, Tuller B (1983) Compensatory articulation under conditions of reduced afferent information: A dynamic formulation. J Speech Hear Res 26: 217-224. Link: https://goo.gl/62M5oh
- Stepp CE, Lester-Smith RA, Abur D, Daliri A, Noordzij JP, et al. (2017) Evidence for auditory-motor impairment in individuals with hyperfunctional voice disorders. J Speech Lang Hear Res 60: 1545-1550. Link: https://goo.gl/Y11Cp7
- Tourville JA, Reilly KJ, Guenther FH (2008) Neural mechanisms underlying auditory feedback control of speech. Neuroimage 39: 1429-1443. Link: https://goo.gl/b6fisD
- Domer AS, Kuhn MA, Belafsky PC (2013) Neuophysiology and clinical implications of the laryngeal adductor reflex. Curr Otorhinolaryngol Rep 1: 178-182. Link: https://goo.gl/G8qw8F
- Aviv JE, Martin JH, Kim T, et al. (1999) Laryngopharyngeal sensory discrimination testing and the laryngeal adductor reflex. Ann Otol Rhinol Laryngol 108: 725-730. Link: https://goo.gl/5vT7zC
- Johnson PE, Belafsky PC, Postma GN (2003) Topical nasal anesthesia and laryngopharyngeal sensory testing: a prospective, double-blind crossover study. Ann Otol Rhinol Laryngol 112: 14-16. Link: https://goo.gl/hrguug
- Morrison M, Rammage L, Emami AJ (1999) The irritable larynx syndrome. J Voice 13: 447-455. Link: https://goo.gl/e81MNH
- Murry T, Branski RC, Yu K, Cukier-Blaj S, Duflo S, et al. (2010) Laryngeal sensory deficits in patients with chronic cough and paradoxical vocal fold movement disorder. Laryngscope 120: 1576-1581. Link: https://goo.gl/mWHhDL
- Lee B, Woo P (2005) Chronic cough as a sign of laryngeal sensory neuropathy: diagnosis and treatment. Ann Otol Rhinol Laryngol 114: 253-257. Link: https://goo.gl/dfDwN6
- Van Mersbergen M, Patrick C, Glaze L (2008) Functional dysphonia during mental imagery: testing the trait theory of voice disorders. J Speech Lang Hear Res 51: 1405-1423. Link: https://goo.gl/g2rvaE
- Roy N, Bless DM, Heisey D (2000) Personality and voice disorder: a multitrait-multidisorder analysis. J Voice 14: 521-548. Link: https://goo.gl/Ye5eW1
- Roy N, Mcgrory JJ, Tasko SM, Bless DM, Heisey D, et al. (1997) Psychological correlates of functional dysphonia: an investigation using the Minnesota multiphasic personality inventory. J Voice 11: 443-451. Link: https://goo.gl/zQpE4G
- Green G (1988) The inter-relationship between vocal and psychological characteristics: a literature review. Aust J Hum Commun Dis 16: 31-43. Link: https://goo.gl/kSkCLt
- Hsiao TY, Liu CM, Hsu CJ, Lee SY, Lin KN (2001) Vocal fold abnormalities in laryngeal tension-fatigue syndrome. J Formos Med Assoc 100: 837-840. Link: https://goo.gl/SoLHuP
- Koufman JA, Blalock PD (1988) Vocal fatigue and dysphonia in the professional voice user: Bogart-Bacall sydrome. Laryngoscope 98: 493-498. Link: https://goo.gl/Ey1PMK
- Sandage MJ, Smith AG (2017) Muscle bioenergetic considerations for intrinsic laryngeal skeletal muscle physiology. J Speech Lang Hear Res 60: 1254-1263. Link: https://goo.gl/YkFU9Q
- Kryshtopava M, Van Lierde K, Meerschman I, et al. (2017) Brain activity during phonation in women with muscle tension dysphonia: An FMRI study. J Voice 3: 10-15. Link: https://goo.gl/5agaCD
- Samargia S, Schmidt R, Kimberley TJ (2016) Cortical silent period reveals differences between adductor spasmodic dysphonia and muscle tension dysphonia. Neurorehabil Neurol Repair 30: 221-232. Link: https://goo.gl/sKkrvM
- Gillespie AI, Gartner-Schmidt J, Rubinstein EN, Abbott KV (2013) Aerodynamic profiles of women with muscle tension dysphonia/aphonia. J Speech Lang Hear Res 56: 481-488. Link: https://goo.gl/43dq7S
- Roy N, Ford CN, Bless DM (1996) Muscle tension dysphonia and spasmodic dysphonia; the role of manual laryngeal tension reduction in diagnosis and management. Ann Otol Rhinol Laryngol 105: 851-856. Link: https://goo.gl/gtR9bH
- Barona-Lleo L, Fernandez S (2016) Hyperfunctional voice disorder in children with attention deficit hyperactivity disorder (ADHD): A phenotypic characteristic? J Voice 30: 114-119. Link: https://goo.gl/Rh2TZU
- D'Alatri L, Petrelli L, Calo L, et al. (2014) Vocal fold nodules in school age children: attention deficit hyperactivity disorder as a potential risk factor. J Voice 7: 19-24. Link: https://goo.gl/Q9aDfP
- Faraone SV, Sergeant J, Gillberg C, Biederman J (2003) The worldwide prevalence of ADHD: is it an American condition? World physchiatry 2: 104-113. Link: https://goo.gl/Q9aDfP
- Van Houtte E, Claeys S, D'Haeseleer E, et al. (2013) An examination of surface EMG for the assessment of muscle tension dysphonia. J Voice 27: 177-186. Link: https://goo.gl/viFpSn
- Stepp CE, Heaton JT, Braden MN, et al. (2011) Comparison of neck tension palpation rating systems with surface electromyographic and acoustic measures in vocal hyperfunction. J Voice 25: 67-75. Link: https://goo.gl/v2N8so
- Hocevar-Boltezar I, Janko M, Zargi M (1987) Roll of surface EMG in diagnostics and treatment of muscle tension dysphonia. Acta Otolaryngol 118: 739-743. Link: https://goo.gl/j2i633
- Wuyts F, De Bodt M, Molenberghs G, et al. (2000) The dysphonia severity index: An objective measure of vocal quality based on a multiparameter approach. J Speech Lang Hear Res 43: 796-809. Link: https://goo.gl/khiQSa
- Jafari N, Salehi A, Izadi F, e al. (2017) Vocal function exercises for a muscles tension dysphonia: auditory-perceptual evaluation and self-assessment rating. J Voice 31: 506-512. Link: https://goo.gl/bp7qz5
- Van Stan JH, Maffei M, Vaz Masson ML, et al. (2017) Self-ratings of vocal status in daily life: Reliability and validity for patients with vocal hyperfunction and a normative group. Am J Speech Lang Path 26: 1167-1177. Link: https://goo.gl/t2MJQt
- Varadarajan V, Blumin JH, Bock JM (2013) State of the art of laryngeal electromyography. Curr Otorhinolaryngol Rep 1: 171-177. Link: https://goo.gl/xoQBTJ
- Prosek RA, Walden BE, Schwartz DM (1978) EMG biofeedback in the treatment of hyperfunctional voice disorders. J Speech Hear Disord 43: 282-294. Link: https://goo.gl/4mEzbo
- Houtz DR, Roy N, Merrill RM, Smith ME (2010) Differential diagnosis of muscle tension dysphonia and adductor spasmodic dysphonia using spectral moments of the long-term average spectrum. Laryngoscope 120: 749-757. Link: https://goo.gl/w7swU3
- Lowell SY, Kelley RT, Colton RH, et al. (2012) Position of the hyoid and larynx in people with muscle tension dysphonia. Laryngoscope 122: 370-377. Link: https://goo.gl/iQ7LXC
- Drake K, Bryans L, Schindler JS (2016) A review of voice therapy techniques employed in treatment of dysphonia with and without vocal fold lesions. Curr Otorhinolaryngol Rep 4: 168-174. Link: https://goo.gl/h4XUU5
- Roy N, Bless D (1998) Manual circumlaryngeal techniques in the assessment and treatment of voice disorders. Curr Opin Otolaryngol Head Neck Surg 6: 151-155. Link: https://goo.gl/EgWesH
- Van Lierde KM, DeBodt M, Dhaeseleer E, et al. (2010) The treatment of muscle tension dysphonia: a comparison of two treatment techniques by means of an objective multiparameter approach. J Voice 24: 294-301. Link: https://goo.gl/hoUmRd
- Gopikishore P, Pushpavathi M (2017) Outcomes of eclectic voice therapy program in the treatment of hyperfunctional voice disorders: a preliminary study. Global J Otolaryngol 8: 001-006. Link: https://goo.gl/42rQ1G
- Wingate JM, Brown WS, Shrivastav R, et al. (2007) Treatment outcomes for professional voice users. J Voice 21: 433-449. Link: https://goo.gl/pMZgc5
- Mathieson L, Hirani SP, Epstein R, et al. (2009) Laryngeal manual therapy: A preliminary study to examine its treatment effects in the management of muscle tension dysphonia. J Voice 23: 353-366. Link: https://goo.gl/RLJBNt
- Sielska-Badurek E, Osuch-Wojcikiewicz E, Sobol M, et al. (2017) Combined functional voice therapy in singers with muscle tension dysphonia in singing. J Voice 31: 509-517. Link: https://goo.gl/QkqE4E
- Craig J, Tomlinson C, Stevens K, et al. (2015) Combining voice therapy and physical therapy: a novel approach to treating muscle tension dysphonia. J Commun Disord 58: 169-178. Link: https://goo.gl/MWMVt5
- Roy N, Leeper HA (1993) Effects of the manual laryngeal musculoskeletal tension reduction technique as a treatment for functional voice disorders: perceptual and acoustic measures. J Voice 3: 242-249. Link: https://goo.gl/mbQ9Z2
- Dominguez LM, Simpson CB (2015) Neurolaryngology: in-office diagnosis and treatment. Curr Otorhinolaryngol Rep 3: 138-143. Link: https://goo.gl/G5VaWj
- Kitago T, Krakauer J (2013) Motor learning principles for neurorehabilitation (Chap 8). In Barnes MP & Good DC (eds): Handbook of Clinical Neurology and Neurological Rehabilitation 110: 93-103. Link: https://goo.gl/AVAMLF
- Dworkin-Valenti JP, Vandjelovic N, Bathula S (2015) The therapeutic value of trans-cricothyroid injections for intractable conversion reaction mutism. Annals of Otolaryngology and Rhinology 2: 1055-1061.
- Dworkin JP (1991) Motor Speech Disorders: A treatment guide book. St. Louis: C.V. Mosby. Link: https://goo.gl/QELriH

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.





 Save to Mendeley
Save to Mendeley
