Archives of Otolaryngology and Rhinology
Obstructive Sleep Apnea Syndrome (OSAS): Who Are Our Patients?
Natália Silva Cavalcanti*, Davi Sandes Sobral, Geísa Pereira Rufino, Lílian da Cruz Lino Salvador, Shirley Santana Santos Correia, Rodrigo Maranhão Marques and Geraldo Druck Sant'anna
Cite this as
Cavalcanti NS (2018) Obstructive Sleep Apnea Syndrome (OSAS): Who Are Our Patients? Arch Otolaryngol Rhinol 4(2): 035-036. DOI: 10.17352/2455-1759.000072Introduction
The Obstructive Sleep Apnea Syndrome (OSAS) is characterized by interruption or reduction of airflow during sleep despite respiratory effort, causing awakenings, oxyhemoglobin desaturation and excessive daytime sleepiness.
It is considered a serious public health problem, according to recent national surveys prevalence up to 30% of the general population, reaching alarming levels [1,2]. OSAS can be undiagnosed in 80% of cases [3].
OSAS is more prevalent in men than women, and there is an increased prevalence among the elderly [1,4]. The prevalence of mild OSAS may vary from 3 to 28% of the adult population, whereas moderate to severe OSAS (AHI>15) may range from 1 to 14% [4].
The factors that increase the risk for OSAS are overweight and obese men and women, age, structural abnormalities in the upper airway, use of sedatives and alcohol, and probably familial history [5]. Long term complications, can lead to important cardiovascular changes, with serious socio-economic implications, deserving medical attention. Snoring, in turn, can significantly interfere in the social life of the patient [6].
The whole-night polysomnography study, which was carried out in the laboratory, is the gold standard method for the diagnosis of sleep disorders. The polysomnographic setting [7], enables the simultaneous registration of several biological variables. Electroencephalogram (EEG), electro-oculogram (EOG), electromyogram (EMG) of the mentalis and limbs, measurements of oronasal flow, thoraco-abdominal movement, electrocardiogram (ECG) and pulse oximetry, are the most commonsigns used among a widesettingvariance of other sensors. Sleep fragmentation due to micro-awakenings secondary to sleep apnea or periodic leg movements may lead to reduced sleep on slow waves and REM [8]. The analysis of these data, faced with the normality standardization, provides us a better understanding of what happens during sleep.
Objective
The aim of this study was to better understand the sleep profile in a group of adults, through the use of polysomnography in a sleep laboratory, in an Otolaryngology Clinic.
Methods
This retrospective study involved data collected from 447 polysomnography tests, which included those from patients over 14 years old, carried out between the years of 2011 and 2014, in an Otorhinolaringology clinic. There were excluded from analysis tests in which the patient had Total Sleep Time (TST) below 120 minutes, and tests with data loss caused by overnight failure of the sensors.
The tests were performed according to AASM Scoring Manual 2007’s standards [9]. The analyzed data were based on age, gender, weight, height, BMI, neck circumference, Epworth Sleepiness Scale, in addition to test motive and the most relevant polysomnographic parameters, such as sleep architecture, sleep Apnea-Hypopnea Index (AHI), presence of snoring and oximetry.
The data were tabulated and the results are distributed, descriptively, in graphs and tables.
Results
The data for age, weight, height, BMI, neck circumference (NC) and Epworth Sleepiness Scale (ESS) were (Table 1):
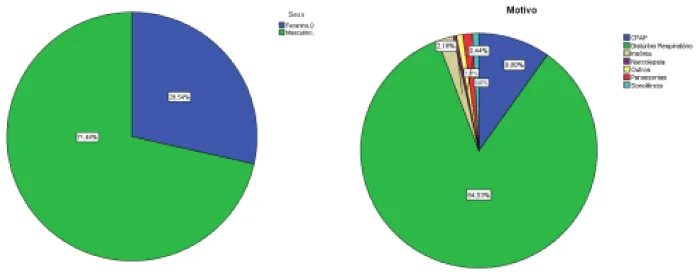
The distribution of patients according to gender and test motivation was (Figure 1):
As to Neurological parameters, it was found (Table 2):
As to respiratory parameters, it was found (Table 3):
Our study evaluate polysomnographies from an ENT clinic. In this way, we concluded that our group was more likely to have respiratory disorders (RD). We have noticed that the main reason for polysomnography requests was due to respiratory disorder, with 84.53% of applications. Males were predominant, with 71.46% of the patients. The mean AHI value of 22.5/h (SD 23.7) was much higher than expected, which corroborated the hypothesis of an existing pathological profile in the group as to sleep RDs [1]. The mean BMI was 28.3 (SD 4.9) which may also have influenced the average AHI, average neck circumference above 40 cm and ESS with an average above 11 points, also sustain the findings attributed to OSAS in the analyzed group and according to many other authors who have pointed in the same direction [10]. Another important aspect to be considered is that our polysomnographies were performed with use of nasal pressure transducer for analysis of respiratory flow, maximizing the detection of hypopneas, other studies used temperature sensors for the detection of obstructive events, known to be less sensitive than pressure transducers [7]. Still under the respiratory point of view, we observed oxyhemoglobin saturation profile reduction in NadirO2 average, 84.9% (SD 10.8), which reinforces the pathological feature of the studied group, corrobarating the increase in the AHI. In this study, as broadly demonstrated in the literature, snoring was an important observed signal. Our patients snored by an average of 28% of total sleep time. Regarding the sleep structure, we point out, as can be seen in table 2, a reduction in the sleep efficiency, in addition to a lower percentage of REM sleep, while the most superficial stages, N1 and N2 had a higher percentage distribution. The reduction standard in deep sleep stages is expected in patients with OSAS, in exchange for a higher percentage of superficial stages. It was observed, similarly, an excessive fragmentation, evidenced by the increased average of arousals index, 24.9/h (SD 17.4). Future comparative analysis related to the data collected in this study will be carried out. We believe the importance for execution prospective studies, as well, improving the standardization of polysomnographic data to better understand the sleep behavior in our patients.
Conclusion
The studied group showed polysomnographic characteristics, both neurological and respiratory, attributed to Obstructive Sleep Apnea Syndrome (OSAS).
- Link: https://tinyurl.com/yadfc4ef
- Thornton AT, Singh P, Ruehland WR, Rochford PD (2012) AASM criteria for scoring respiratory events: interaction between apnea sensor and hypopnea definition. Sleep 35: 425-432. Link: https://tinyurl.com/y7b25b69
- Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle aged men and women. Sleep 20: 705-706. Link: https://tinyurl.com/ya2sm5gw
- Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165: 1217-1239. Link: https://tinyurl.com/y72x2r49
- Mendes FA, Marone SAM, Duarte BB, Arenas ACP (2014) Epidemiologic Profile of Patients with Snoring and Obstructive Sleep Apnea in a University Hospital. Int Arch Otorhinolaryngol 18: 142-145. Link: https://tinyurl.com/ycnt9j2l
- Bozkurt NC, Beysel S, Karbek B, Unsal IO, Cakir E, et al. (2016) Visceral Obesity Mediates the Association Between Metabolic Syndrome and Obstructive Sleep Apnea Syndrome. Metab Syndr Relat Disord. 14: 217-221. Link: https://tinyurl.com/y887w8f5
- Ayappa I, Norman RG, Krieger AC, Rosen A, O'malley RL, et al. (2000) Non-Invasive detection of respiratory effort-related arousals (REras) by a nasal cannula/ pressure transducer system. Sleep. 23: 763-71. Link: https://tinyurl.com/yaa7599y
- Togeiro SM, Smith AK (2005) Diagnostics methods for sleep disorders. Rev Bras Psiquiatr 27: 8-15. Link: https://tinyurl.com/y7a8ayno
- Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, et al. (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. American Academy of Sleep Medicine. J Clin Sleep Med 8: 597-619. Link: https://tinyurl.com/ycf4urut
- Canani SF, Menna Barreto SS (2001) Sleepiness and automobile accidents. J Pneumol 27: 946.

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
