Archives of Otolaryngology and Rhinology
Four cases of extracranial abscess caused by sinusitis exacerbated by a foreign body
Kazuhiro Takahashi and Muneo Nakaya*
Cite this as
Takahashi K, Nakaya M (2018) Four cases of extracranial abscess caused by sinusitis exacerbated by a foreign body. Arch Otolaryngol Rhinol 4(3): 050-052. DOI: 10.17352/2455-1759.000076Background: Foreign bodies in the paranasal sinus is a relatively rare. Furthermore, most of foreign bodies in the paranasal sinuses occur in the maxillary sinus, and reports of foreign bodies in frontal sinus are few. Extracranial abscesses caused by sinusitis with foreign bodies is a rare, but it sometimes cause serious complications. We report four cases of extracranial abscess caused by sinusitis exacerbated by a foreign body.
Case report: In all four cases, temporal subcutaneous abscess developed 10 or more years after receiving craniotomy. A CT scan revealed the frontal sinus had traffic to the plate and a subcutaneous abscess was observed around the plate. In three cases, a drainage route was created by endoscopic sinus surgery, and in two cases, Draf type Ⅲ was performed. However, the infection due to foreign matter did not improve, and it cured by removing residual foreign matter. In one case, symptoms were improved by creating a drainage route, and removal of foreign matter was unnecessary.
Conclusion: Infection of the frontal sinuses by a foreign body requires the creation of a drainage route, although it is sometimes necessary to remove the foreign body if the infection continues even after drainage.
Introduction
Cases of foreign bodies in the paranasal sinus are relatively rare because the paranasal sinuses are surrounded by bone. Furthermore, most foreign bodies in the paranasal sinuses occur in the maxillary sinus, and reports of foreign bodies in the frontal sinus are few [1]. We experienced four cases of extracranial abscess without osteomyelitis caused by sinusitis exacerbated by a foreign body and review some of the relevant literature.
Case Report
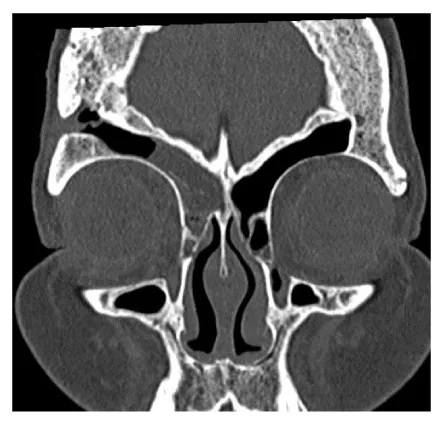
Case 1: A 68-year-old woman with a medical history which included rheumatoid arthritis, Sjogren's syndrome, diabetes, and hypertension underwent a craniotomy for subarachnoid hemorrhage in October 1991. In November 2007, she underwent right endoscopic surgery for purulent discharge from the right nasal cavity at another hospital. Two days after the operation, a right temporal subcutaneous abscess and right orbital abscess developed. Endoscopic sinus surgery was performed to drain the abscess, and a tube was placed in the nasofrontal duct. Thereafter, the inflammation improved, but the right temporal subcutaneous abscess recurred. She was referred to the neurosurgery department of our hospital in April 2008. Although she was followed up as an outpatient and underwent incisional drainage, the subcutaneous abscess recurred multiple times. Treatment for chronic frontal sinusitis was considered necessary to improve the right temporal subcutaneous abscess, and she was referred to our department in December 2008. At the first visit, she presented a discharge of pus from the right forehead. A CT scan revealed soft tissue density in the right frontal sinus and ethmoid sinus (Figure 1). We performed an endoscopic modified Lothrop procedure (Draf Ⅲ) for frontal sinus surgery in January 2009 [1]. An artifact thought to be the source of infection, was removed from the back of the frontal sinus and turned out to be resin used in a craniotomy. Because of the hardness, it was impossible to remove the object endoscopically. After endoscopic sinus surgery, the purulent rhinorrhea improved, but discharge of pus from the temporal subcutaneous abscesses did not. In March 2009, the foreign body was removed by extracranial surgery in the department of neurosurgery. After the surgery, debridement for the postoperative infection was performed in the department of plastic surgery. The postoperative course was uneventful.
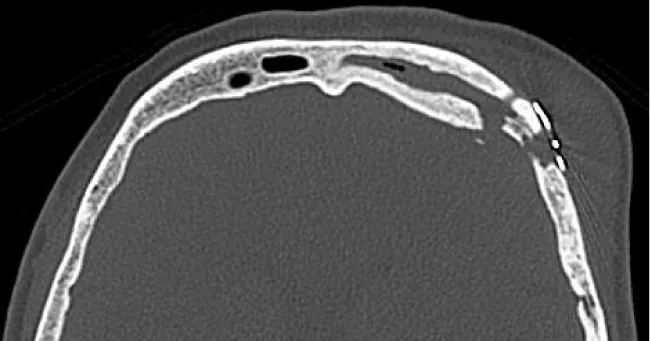
Case 2: A 60-year-old female with a medical history that included cerebral aneurysm, bronchiectasis, and rheumatoid arthritis underwent a craniotomy for cerebral aneurysms in 2005. Sinusitis was pointed out at the time. After the craniotomy, she continued to have chronic purulent nasal discharge and occasional pain. In April 2014 the pain and swelling in the left forehead gradually worsened. She visited our neurosurgery department and was referred to our department for the treatment of sinusitis. At the first visit, she had a swelling and tenderness in the left forehead. A CT scan revealed left paranasal sinusitis; the left frontal sinus had traffic to the plate and a subcutaneous abscess was observed around the plate (Figure 2). In May 2014, left endoscopic sinus surgery and left anterior temporal incisional drainage were performed. A large amount of exudates was observed when the site of swelling in the left frontal region was incised and the plate was exposed. Although washing treatment was done daily, discharge of the pus from the temporal subcutaneous abscess did not improve due to the infected granulation tissue around the metal plate. She underwent debridement and plate removal in the department of plastic surgery and department of neurosurgery. The postoperative course was uneventful.
Case 3: A 74-year-old female with a medical history which included dyslipidemias, osteoporosis, cataracts, and appendicitis underwent a craniotomy after falling off her bicycle in September 2000. In December 2014, she presented a fistula in the left forehead with discharge of pus, and received the diagnosis of postoperative epidural abscess. In March 2015, autogenous bone removal and debridement were performed at the neurosurgery department of our hospital. However, in August 2015 she was referred our department due to the recurrence of fistula, discharge of pus, and swelling of the left forehead.
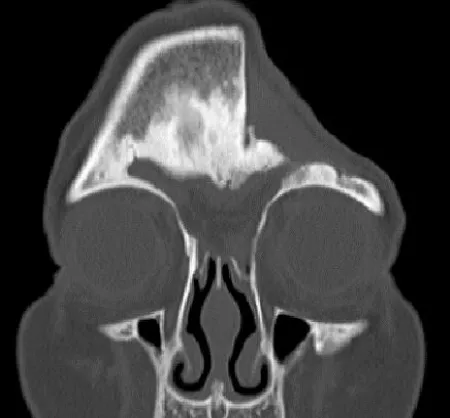
At the first visit, she presented discharge of pus from the fistula in the bone defect of the left forehead. A CT scan revealed a frontal sinus septal defect and the frontal sinus filled with a soft tissue density mass (Figure 3). We performed an endoscopic modified Lothrop procedure (Draf Ⅲ) for frontal sinus surgery in October 2015. The resin injected during surgery for the head injury and pus were found in the left frontal sinus. We removed the resin completely. The postoperative course was uneventful.
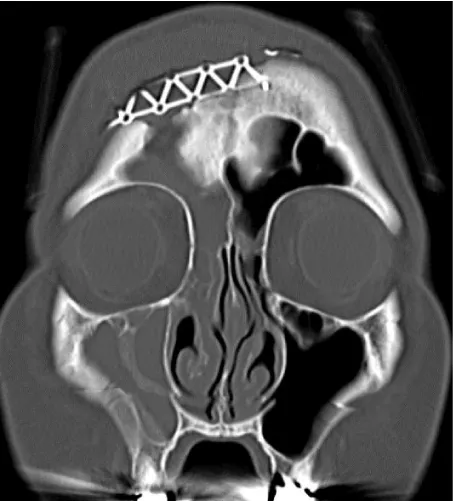
Case 4: A 58-year-old female with a medical history that included uterine fibroids and hypertension underwent a craniotomy for a subarachnoid hemorrhage in June 2005. She experienced right paralysis as a sequela. In March 2017, she experienced a swelling of the forehead and received the diagnosis of subcutaneous abscess in the forehead by CT scan. She was referred our department. At the first visit, swelling with tenderness was noted in the forehead. A CT scan revealed a right upper 7th apical lesion, right sinusitis, and subcutaneous abscess over the titanium plate. The right frontal sinus had traffic to the titanium plate (Figure 4). Right odontogenic maxillary sinusitis was thought to have spread to the titanium plate of the right frontal sinus, and in March 2017, right endoscopic sinus surgery and incisional drainage for the subcutaneous abscess in the forehead were performed. A large amount of exudates drained out when the site of swelling in the forehead was excised, and the titanium plate was exposed. Daily washing was performed. Because there was no sign of infection, the wound was closed. The postoperative course was uneventful.
Discussion
In the present four cases, frontal sinusitis and infection around the foreign body occurred more than ten years after the craniotomy. In these cases, part of the wall of the frontal sinus was deformed due to the craniotomy, resulting in traffic with the foreign body. Therefore, it was thought that the sinusitis was the first route of infection, which then spread around the foreign body through the defect in the frontal sinus wall. Also, the foreign body infection occurred ten years after the craniotomy in case 1 due to the patient's diabetes and her regimen of PSL 3 mg / day for rheumatoid arthritis. In case 2, the patient had been taking an immunosuppressive agent for rheumatoid arthritis. In case 3, the patient was elderly. Therefore, we believe that the presence of the foreign body led to infection due to a gradual compromising of the patient's health over the course of more than 10 years.
As treatment, in addition to antibiotic administration, abscess drainage and aeration of the frontal sinus by surgery were required. Surgery for frontal sinusitis includes the endoscopic nasal method, the extranasal method with an external incision, and the combination of the intranasal method and the extranasal method. Since it is anatomically difficult to observe the frontal sinus from inside the nose, the extranasal method used to be performed frequently, but due to the development of endoscopes and surgical instruments in recent years, the nasal method is being used more often. The intranasal method, which is less invasive and cosmetically superior, should be the first choice, and in cases in which the approach to the frontal sinus is difficult using the intranasal method, the extranasal method should be chosen. If the frontal sinus can be opened to the nasal cavity widely enough, frontal sinusitis can be cured. However, in cases in which stenosis or obstruction after surgery is a possibility due to an insufficiently open frontal sinus, good results were reportedly obtained by placing a silicon tube in the drainage route [2]. Draf type Ⅲ, which removes the nasal septum and the frontal sinus septum and unifies the frontal sinus by connecting the right and left frontal sinus ostium openings, can create a large drainage route from the frontal sinus to the nasal cavity and is becoming a standard surgical procedure for refractory frontal sinusitis and frontal sinus cyst [2].
In case 1, although the endoscopic sinus surgery was performed at other hospitals, the right temporal subcutaneous abscess recurred after surgery. In order to open the frontal sinuses more widely, we performed Draf type Ⅲ. During surgery, we found resin in the frontal sinus, which was identified as the source of the infection.
Artificial resin (mainly methacrylic resin) was used as a filling material in cranioplasty surgery. It was often used in the past because it can be molded to any size or shape, and there are few artifacts on CT or MRI [3]. Currently, it is almost never used due to its durability and likelihood to cause infection, and titanium is now the preferred material. Although the discharge of pus from the fistula continued even after Draf type Ⅲ in case1, the infection was able to be controlled by removing the resin. In case 2, the drainage route was created by left endoscopic sinus surgery and left anterior temporal incision drainage, but the infected granulation tissue over the metal plate was able to be healed only by removing the metal plate. In case 3, foreign body (autogenous bone) removal and debridement were performed at the neurosurgery department, but drainage of pus from the fistula recurred and was able to be improved by Draf type Ⅲ and removal of the residual foreign body in the frontal sinus. In case 4, right odontogenic maxillary sinusitis was thought to have spread to the titanium plate of the right frontal sinus, and a drainage route was created by right endoscopic sinus surgery with incisional drainage of the subcutaneous abscess in the forehead. As a result, symptoms improved and removal of the foreign body was unnecessary.
In summary, infection of the frontal sinuses by a foreign body requires the creation of a drainage route although it is sometimes necessary to remove the foreign body if the infection continues even after drainage. Frontal sinusitis caused by a foreign body is rare, but sometimes causes serious complications. If patients have a medical history of intracranial surgery, the possibility of a foreign body infection should be considered.
Conclusion
We reported four cases of extracranial abscess caused by sinusitis exacerbated by a foreign body.
- (2009) Sedat AYDIN: Glass Particles in the Frontal Sinus: Turk J Med Sci 39: 313-315. Link: https://tinyurl.com/ycyqxw4x
- Kikawada T, Fujigaki M, Kikura M, Matsumoto M, Kikawada K (1999) Extended endoscopic frontal sinus surgery to interrupted nasofrontal communication caused by scarring of the anterior ethmoid: long-term results. Arch Otolaryngol Head Neck Surg 125: 92-96. Link: https://tinyurl.com/y7ttnmn6
- Morioka T, Fujiwara S, Akimoto T, Nishio S, Fukui M (1996) Intracranial epidural abscess: late complication of allograft cranioplasty. Fukuoka Igaku Zasshi 87: 57-59. Link: https://tinyurl.com/y9ar4vqx

Article Alerts
Subscribe to our articles alerts and stay tuned.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.
 Save to Mendeley
Save to Mendeley
